当前位置:
X-MOL 学术
›
J. Allergy Clin. Immunol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
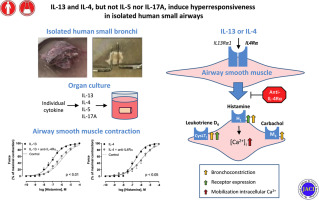
IL-13 and IL-4, but not IL-5 nor IL-17A, induce hyperresponsiveness in isolated human small airways.
Journal of Allergy and Clinical Immunology ( IF 11.4 ) Pub Date : 2019-12-02 , DOI: 10.1016/j.jaci.2019.10.037 Martijn L Manson 1 , Jesper Säfholm 2 , Anna James 2 , Anna-Karin Johnsson 2 , Per Bergman 3 , Mamdoh Al-Ameri 3 , Ann-Charlotte Orre 4 , Carina Kärrman-Mårdh 5 , Sven-Erik Dahlén 2 , Mikael Adner 2
Journal of Allergy and Clinical Immunology ( IF 11.4 ) Pub Date : 2019-12-02 , DOI: 10.1016/j.jaci.2019.10.037 Martijn L Manson 1 , Jesper Säfholm 2 , Anna James 2 , Anna-Karin Johnsson 2 , Per Bergman 3 , Mamdoh Al-Ameri 3 , Ann-Charlotte Orre 4 , Carina Kärrman-Mårdh 5 , Sven-Erik Dahlén 2 , Mikael Adner 2
Affiliation
|
BACKGROUND
Specific inflammatory pathways are indicated to contribute to severe asthma, but their individual involvement in the development of airway hyperresponsiveness remains unexplored.
OBJECTIVE
This experimental study in human small bronchi aimed to provide insight into which of the type 2 and type 17 cytokines cause hyperresponsiveness of airway smooth muscle.
METHODS
Explanted small bronchi isolated from human lung tissue and human airway smooth muscle cells were treated for 2 and 1 day(s), respectively, with 100 ng/mL of IL-4, IL-5, IL-13, or IL-17A, and contractile responses, Ca2+ mobilization, and receptor expression were assessed.
RESULTS
Treatment with IL-13 increased the potency of histamine, carbachol, and leukotriene D4 as contractile agonists. IL-4, but not IL-5 or IL-17A, also increased the potency of histamine. In human airway smooth muscle cells, IL-13 and IL-4, but not IL-5 and IL-17A, enhanced the histamine-induced Ca2+ mobilization that was accompanied with increased mRNA expression of histamine H1 and cysteinyl leukotriene CysLT1 receptors. RNA sequencing of isolated bronchi confirmed the IL-13-mediated upregulation of H1 and CysLT1 receptors, without showing an alteration of muscarinic M3 receptors. Dexamethasone had no effects on IL-13-induced hyperresponsiveness in human bronchi, the increased Ca2+ mobilization, or the enhanced receptor expression. In contrast, antagonism of the common receptor for IL-13 and IL-4 by the biologic dupilumab prevented the effects of both IL-13 and IL-4 in human bronchi and human airway smooth muscle cells.
CONCLUSIONS
The glucocorticoid-insensitive hyperrresponsiveness in isolated human airways induced by IL-13 and IL-4 provides further evidence that the IL-4Rα pathway should be targeted as a new strategy for the treatment of airway hyperresponsiveness in asthma.
中文翻译:

IL-13 和 IL-4,但不是 IL-5 和 IL-17A,在孤立的人类小气道中诱导高反应性。
背景 指出特定的炎症途径会导致严重的哮喘,但它们在气道高反应性发展中的个体参与仍有待探索。目的 本项人类小支气管实验研究旨在深入了解 2 型和 17 型细胞因子中的哪一种会导致气道平滑肌的高反应性。方法 从人肺组织和人气道平滑肌细胞中分离的外植小支气管分别用 100 ng/mL IL-4、IL-5、IL-13 或 IL-17A 处理 2 天和 1 天,并评估了收缩反应、Ca2+ 动员和受体表达。结果 用 IL-13 治疗增加了组胺、氨甲酰胆碱和白三烯 D4 作为收缩激动剂的效力。IL-4,但不是 IL-5 或 IL-17A,也增加了组胺的效力。在人气道平滑肌细胞中,IL-13 和 IL-4,而不是 IL-5 和 IL-17A,增强了组胺诱导的 Ca2+ 动员,伴随着组胺 H1 和半胱氨酰白三烯 CysLT1 受体的 mRNA 表达增加。分离的支气管的 RNA 测序证实了 IL-13 介导的 H1 和 CysLT1 受体的上调,但没有显示毒蕈碱 M3 受体的改变。地塞米松对 IL-13 诱导的人支气管高反应性、增加的 Ca2+ 动员或增强的受体表达没有影响。相比之下,生物制品 dupilumab 对 IL-13 和 IL-4 的共同受体的拮抗作用阻止了 IL-13 和 IL-4 在人支气管和人气道平滑肌细胞中的作用。
更新日期:2019-12-02
中文翻译:

IL-13 和 IL-4,但不是 IL-5 和 IL-17A,在孤立的人类小气道中诱导高反应性。
背景 指出特定的炎症途径会导致严重的哮喘,但它们在气道高反应性发展中的个体参与仍有待探索。目的 本项人类小支气管实验研究旨在深入了解 2 型和 17 型细胞因子中的哪一种会导致气道平滑肌的高反应性。方法 从人肺组织和人气道平滑肌细胞中分离的外植小支气管分别用 100 ng/mL IL-4、IL-5、IL-13 或 IL-17A 处理 2 天和 1 天,并评估了收缩反应、Ca2+ 动员和受体表达。结果 用 IL-13 治疗增加了组胺、氨甲酰胆碱和白三烯 D4 作为收缩激动剂的效力。IL-4,但不是 IL-5 或 IL-17A,也增加了组胺的效力。在人气道平滑肌细胞中,IL-13 和 IL-4,而不是 IL-5 和 IL-17A,增强了组胺诱导的 Ca2+ 动员,伴随着组胺 H1 和半胱氨酰白三烯 CysLT1 受体的 mRNA 表达增加。分离的支气管的 RNA 测序证实了 IL-13 介导的 H1 和 CysLT1 受体的上调,但没有显示毒蕈碱 M3 受体的改变。地塞米松对 IL-13 诱导的人支气管高反应性、增加的 Ca2+ 动员或增强的受体表达没有影响。相比之下,生物制品 dupilumab 对 IL-13 和 IL-4 的共同受体的拮抗作用阻止了 IL-13 和 IL-4 在人支气管和人气道平滑肌细胞中的作用。








































 京公网安备 11010802027423号
京公网安备 11010802027423号