Computational and Structural Biotechnology Journal ( IF 4.4 ) Pub Date : 2020-01-17 , DOI: 10.1016/j.csbj.2020.01.002 Sundeep Chaitanya Vedithi 1 , Carlos H M Rodrigues 2, 3 , Stephanie Portelli 2, 3 , Marcin J Skwark 1 , Madhusmita Das 4 , David B Ascher 1, 2, 3 , Tom L Blundell 1 , Sony Malhotra 1
|
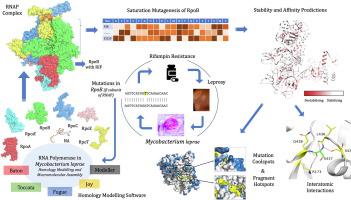
Rifampin resistance in leprosy may remain undetected due to the lack of rapid and effective diagnostic tools. A quick and reliable method is essential to determine the impacts of emerging detrimental mutations in the drug targets. The functional consequences of missense mutations in the β-subunit of RNA polymerase (RNAP) in Mycobacterium leprae (M. leprae) contribute to phenotypic resistance to rifampin in leprosy. Here, we report in-silico saturation mutagenesis of all residues in the β-subunit of RNAP to all other 19 amino acid types (generating 21,394 mutations for 1126 residues) and predict their impacts on overall thermodynamic stability, on interactions at subunit interfaces, and on β-subunit-RNA and rifampin affinities (only for the rifampin binding site) using state-of-the-art structure, sequence and normal mode analysis-based methods. Mutations in the conserved residues that line the active-site cleft show largely destabilizing effects, resulting in increased relative solvent accessibility and a concomitant decrease in residue-depth (the extent to which a residue is buried in the protein structure space) of the mutant residues. The mutations at residue positions S437, G459, H451, P489, K884 and H1035 are identified as extremely detrimental as they induce highly destabilizing effects on the overall protein stability, and nucleic acid and rifampin affinities. Destabilizing effects were predicted for all the clinically/experimentally identified rifampin-resistant mutations in M. leprae indicating that this model can be used as a surveillance tool to monitor emerging detrimental mutations that destabilise RNAP-rifampin interactions and confer rifampin resistance in leprosy.
Author summary
The emergence of primary and secondary drug resistance to rifampin in leprosy is a growing concern and poses a threat to the leprosy control and elimination measures globally. In the absence of an effective in-vitro system to detect and monitor phenotypic resistance to rifampin in leprosy, diagnosis mainly relies on the presence of mutations in drug resistance determining regions of the rpoB gene that encodes the β-subunit of RNAP in M. leprae. Few labs in the world perform mouse footpad propagation of M. leprae in the presence of drugs (rifampin) to determine growth patterns and confirm resistance, however the duration of these methods lasts from 8 to 12 months making them impractical for diagnosis. Understanding molecular mechanisms of drug resistance is vital to associating mutations to clinically detected drug resistance in leprosy. Here we propose an in-silico saturation mutagenesis approach to comprehensively elucidate the structural implications of any mutations that exist or that can arise in the β-subunit of RNAP in M. leprae. Most of the predicted mutations may not occur in M. leprae due to fitness costs but the information thus generated by this approach help decipher the impacts of mutations across the structure and conversely enable identification of stable regions in the protein that are least impacted by mutations (mutation coolspots) which can be a potential choice for small molecule binding and structure guided drug discovery.
中文翻译:

计算饱和诱变预测麻风分枝杆菌 RNA 聚合酶 β 亚基系统突变的结构后果。
由于缺乏快速有效的诊断工具,麻风病对利福平的耐药性可能仍未被发现。一种快速可靠的方法对于确定药物靶标中新出现的有害突变的影响至关重要。麻风分枝杆菌( M. leprae )中 RNA 聚合酶 (RNAP) 的 β 亚基错义突变的功能后果有助于麻风病患者对利福平的表型耐药。在这里,我们在计算机上报告RNAP β-亚基中的所有残基向所有其他 19 种氨基酸类型进行饱和诱变(对 1126 个残基产生 21,394 个突变),并预测它们对整体热力学稳定性、亚基界面相互作用以及 β-亚基-RNA 和利福平亲和力(仅针对利福平结合位点)使用最先进的基于结构、序列和正态模式分析的方法。沿着活性位点裂缝排列的保守残基中的突变显示出很大程度上不稳定的影响,导致相对溶剂可及性增加,并伴随突变残基的残基深度(残基埋在蛋白质结构空间中的程度)降低. 残基位置 S437、G459、H451、P489、K884 和 H1035 被认为是极其有害的,因为它们会对整体蛋白质稳定性以及核酸和利福平的亲和力产生高度不稳定的影响。预测了所有临床/实验鉴定的利福平耐药突变的不稳定效应M. leprae表明该模型可用作监测工具,以监测新出现的有害突变,这些突变破坏了 RNAP-利福平相互作用并在麻风病中赋予利福平耐药性。
作者总结
麻风病患者对利福平的原发性和继发性耐药性日益引起关注,并对全球麻风病控制和消除措施构成威胁。在缺乏有效的体外系统来检测和监测麻风病患者对利福平的表型耐药性的情况下,诊断主要依赖于编码麻风杆菌中 RNAP β 亚基的rpoB基因的耐药决定区是否存在突变. 世界上很少有实验室进行麻风杆菌的小鼠足垫繁殖在存在药物(利福平)的情况下确定生长模式并确认耐药性,但这些方法的持续时间为 8 至 12 个月,因此无法用于诊断。了解耐药性的分子机制对于将突变与临床检测到的麻风病耐药性相关联至关重要。在这里,我们提出了一种计算机饱和诱变方法,以全面阐明在麻风杆菌中 RNAP 的 β 亚基中存在或可能出现的任何突变的结构含义。大多数预测的突变可能不会发生在麻风杆菌中由于适应度成本,但由此产生的信息有助于破译突变对整个结构的影响,相反,能够识别蛋白质中受突变影响最小的稳定区域(突变冷却点),这可能是小分子的潜在选择结合和结构指导的药物发现。











































 京公网安备 11010802027423号
京公网安备 11010802027423号