当前位置:
X-MOL 学术
›
Modern Pathol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Clinicopathological significance of deficient DNA mismatch repair and MLH1 promoter methylation in endometrioid endometrial carcinoma.
Modern Pathology ( IF 7.1 ) Pub Date : 2020-02-14 , DOI: 10.1038/s41379-020-0501-8 Annukka Pasanen 1, 2 , Mikko Loukovaara 3 , Ralf Bützow 1, 2, 3
Modern Pathology ( IF 7.1 ) Pub Date : 2020-02-14 , DOI: 10.1038/s41379-020-0501-8 Annukka Pasanen 1, 2 , Mikko Loukovaara 3 , Ralf Bützow 1, 2, 3
Affiliation
|
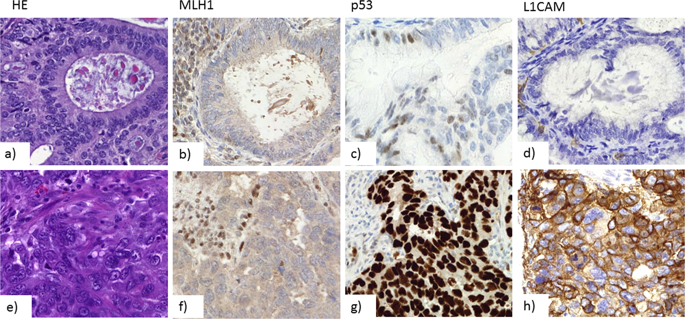
The pathogenesis of DNA mismatch repair (MMR)-deficient endometrial carcinoma (EC) is driven by inactivating methylation or less frequently mutation of an MMR gene (MLH1, PMS2, MSH2, or MSH6). This study evaluated the prognostic and clinicopathologic differences between methylation-linked and nonmethylated MMR-deficient endometrioid ECs. We performed MMR immunohistochemistry and methylation-specific multiplex ligation-dependent probe amplification, and classified 682 unselected endometrioid ECs as MMR proficient (MMRp, n = 438) and MMR deficient (MMRd, n = 244), with the latter subcategorized as methylated (MMRd Met) and nonmethylated tumors. Loss of MMR protein expression was detected in 35.8% of the tumors as follows: MLH1 + PMS2 in 29.8%, PMS2 in 0.9%, MSH2 + MSH6 in 1.3%, MSH6 in 2.8%, and multiple abnormalities in 0.9%. Of the 244 MMRd cases, 76% were methylation-linked. MMR deficiency was associated with older age, high grade of differentiation (G3), advanced stage (II-IV), larger tumor size, abundant tumor-infiltrating lymphocytes, PD-L1 positivity in immune cells and combined positive score, wild-type p53, negative L1CAM, ARID1A loss, and type of adjuvant therapy. MMRd-Met phenotype correlated with older age and larger tumor size, and predicted diminished disease-specific survival in the whole cohort. In the MMRd subgroup, univariate analysis demonstrated an association between disease-specific survival and disease stage II-IV, high grade (G3), deep myometrial invasion, lymphovascular invasion, ER negativity, and L1CAM positivity. In conclusion, MMR methylation profile correlates with clinicopathologic characteristics of endometrioid EC, and MMRd-Met phenotype predicts lower disease-specific survival. MMR deficiency, but not MLH1 methylation status, correlates with T-cell inflammation and PD-L1 expression.
中文翻译:

子宫内膜样子宫内膜癌中 DNA 错配修复缺陷和 MLH1 启动子甲基化的临床病理学意义。
DNA 错配修复 (MMR) 缺陷型子宫内膜癌 (EC) 的发病机制是由甲基化失活或 MMR 基因(MLH1、PMS2、MSH2 或 MSH6)的不太频繁的突变驱动的。本研究评估了甲基化相关和非甲基化 MMR 缺陷型子宫内膜样 EC 之间的预后和临床病理学差异。我们进行了 MMR 免疫组织化学和甲基化特异性多重连接依赖性探针扩增,并将 682 个未选择的子宫内膜样 EC 分类为 MMR 熟练(MMRp,n = 438)和 MMR 缺陷(MMRd,n = 244),后者被子分类为甲基化(MMRd Met) 和非甲基化肿瘤。在 35.8% 的肿瘤中检测到 MMR 蛋白表达缺失,如下所示:MLH1 + PMS2 占 29.8%,PMS2 占 0.9%,MSH2 + MSH6 占 1.3%,MSH6 占 2.8%,多重异常占 0.9%。在 244 例 MMRd 病例中,76% 是甲基化相关的。MMR 缺陷与年龄较大、分化程度高 (G3)、晚期 (II-IV)、肿瘤较大、肿瘤浸润淋巴细胞丰富、免疫细胞 PD-L1 阳性和综合阳性评分、野生型 p53 相关、L1CAM 阴性、ARID1A 丢失和辅助治疗的类型。MMRd-Met 表型与年龄较大和较大的肿瘤大小相关,并预测整个队列中疾病特异性存活率下降。在 MMRd 亚组中,单变量分析表明疾病特异性生存与疾病 II-IV 期、高级别 (G3)、深层肌层浸润、淋巴血管浸润、ER 阴性和 L1CAM 阳性之间存在关联。总之,MMR 甲基化谱与子宫内膜样 EC 的临床病理特征相关,MMRd-Met 表型预测较低的疾病特异性存活率。MMR 缺陷,而非 MLH1 甲基化状态,与 T 细胞炎症和 PD-L1 表达相关。
更新日期:2020-02-14
中文翻译:

子宫内膜样子宫内膜癌中 DNA 错配修复缺陷和 MLH1 启动子甲基化的临床病理学意义。
DNA 错配修复 (MMR) 缺陷型子宫内膜癌 (EC) 的发病机制是由甲基化失活或 MMR 基因(MLH1、PMS2、MSH2 或 MSH6)的不太频繁的突变驱动的。本研究评估了甲基化相关和非甲基化 MMR 缺陷型子宫内膜样 EC 之间的预后和临床病理学差异。我们进行了 MMR 免疫组织化学和甲基化特异性多重连接依赖性探针扩增,并将 682 个未选择的子宫内膜样 EC 分类为 MMR 熟练(MMRp,n = 438)和 MMR 缺陷(MMRd,n = 244),后者被子分类为甲基化(MMRd Met) 和非甲基化肿瘤。在 35.8% 的肿瘤中检测到 MMR 蛋白表达缺失,如下所示:MLH1 + PMS2 占 29.8%,PMS2 占 0.9%,MSH2 + MSH6 占 1.3%,MSH6 占 2.8%,多重异常占 0.9%。在 244 例 MMRd 病例中,76% 是甲基化相关的。MMR 缺陷与年龄较大、分化程度高 (G3)、晚期 (II-IV)、肿瘤较大、肿瘤浸润淋巴细胞丰富、免疫细胞 PD-L1 阳性和综合阳性评分、野生型 p53 相关、L1CAM 阴性、ARID1A 丢失和辅助治疗的类型。MMRd-Met 表型与年龄较大和较大的肿瘤大小相关,并预测整个队列中疾病特异性存活率下降。在 MMRd 亚组中,单变量分析表明疾病特异性生存与疾病 II-IV 期、高级别 (G3)、深层肌层浸润、淋巴血管浸润、ER 阴性和 L1CAM 阳性之间存在关联。总之,MMR 甲基化谱与子宫内膜样 EC 的临床病理特征相关,MMRd-Met 表型预测较低的疾病特异性存活率。MMR 缺陷,而非 MLH1 甲基化状态,与 T 细胞炎症和 PD-L1 表达相关。











































 京公网安备 11010802027423号
京公网安备 11010802027423号