当前位置:
X-MOL 学术
›
Acta Pharmacol. Sin.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Platelet microparticles contribute to aortic vascular endothelial injury in diabetes via the mTORC1 pathway.
Acta Pharmacologica Sinica ( IF 6.9 ) Pub Date : 2018-Nov-16 , DOI: 10.1038/s41401-018-0186-4 Gui-hua Wang , Kun-ling Ma , Yang Zhang , Ze-bo Hu , Liang Liu , Jian Lu , Pei-pei Chen , Chen-chen Lu , Xiong-zhong Ruan , Bi-cheng Liu
Acta Pharmacologica Sinica ( IF 6.9 ) Pub Date : 2018-Nov-16 , DOI: 10.1038/s41401-018-0186-4 Gui-hua Wang , Kun-ling Ma , Yang Zhang , Ze-bo Hu , Liang Liu , Jian Lu , Pei-pei Chen , Chen-chen Lu , Xiong-zhong Ruan , Bi-cheng Liu
|
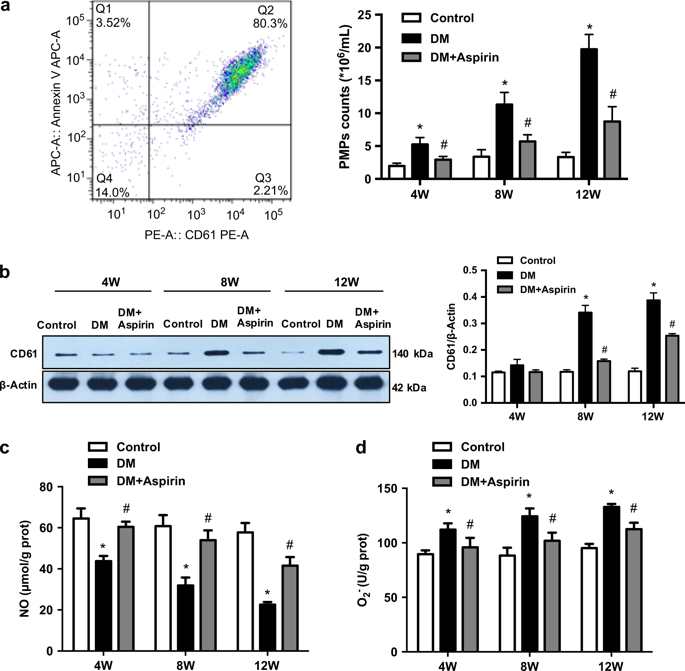
Platelet microparticles (PMPs) are closely associated with diabetic macrovascular complications. The present study aimed to investigate the effects of PMPs in diabetes on aortic vascular endothelial injury and to explore the underlying mechanisms. Peritoneal injection of streptozotocin was used to generate a diabetic rat model in vivo, and human umbilical vein endothelial cells (HUVECs) treated with PMPs were used in vitro. PMP levels in the circulation and aorta tissues were time-dependently increased in streptozotocin-induced diabetic rats at weeks 4, 8, and 12 (P < 0.05). Aspirin significantly inhibited the PMP levels at each time point (P < 0.05). In diabetic rats, the endothelial nitric oxide levels were decreased significantly combined with increased endothelial permeability. PMPs were internalized by HUVECs and primarily accumulated around the nuclei. PMPs inhibited endothelial nitric oxide levels to about 50% and caused approximately twofold increase in reactive oxygen species production. Furthermore, PMPs significantly decreased the endothelial glycocalyx area and expression levels of glypican-1 and occludin (P < 0.05). Interestingly, the PMP-induced endothelial injuries were prevented by raptor siRNA and rapamycin. In conclusion, increased PMPs levels contribute to aortic vascular endothelial injuries in diabetes through activating the mTORC1 pathway.
中文翻译:

血小板微粒通过mTORC1途径促成糖尿病的主动脉血管内皮损伤。
血小板微粒(PMP)与糖尿病大血管并发症密切相关。本研究旨在探讨糖尿病患者中PMPs对主动脉血管内皮损伤的影响并探讨其潜在机制。腹膜内注射链脲佐菌素可在体内产生糖尿病大鼠模型,体外使用经PMP处理的人脐静脉内皮细胞(HUVEC)。在链脲佐菌素诱导的糖尿病大鼠中,在第4、8和12周时,循环和主动脉组织中的PMP水平呈时间依赖性增加(P <0.05)。阿司匹林在每个时间点均显着抑制PMP水平(P <0.05)。在糖尿病大鼠中,内皮一氧化氮水平显着降低,同时内皮通透性增加。PMP被HUVEC内在化,并主要聚集在细胞核周围。PMP将内皮一氧化氮水平抑制到约50%,并导致活性氧的产生增加约两倍。此外,PMPs显着降低了内皮糖萼的面积以及glypican-1和occludin的表达水平(P <0.05)。有趣的是,猛禽siRNA和雷帕霉素可预防PMP诱导的内皮损伤。总之,增加的PMPs水平通过激活mTORC1途径导致糖尿病主动脉血管内皮损伤。PMPs显着降低了内皮糖萼面积以及glypican-1和occludin的表达水平(P <0.05)。有趣的是,猛禽siRNA和雷帕霉素可预防PMP诱导的内皮损伤。总之,增加的PMPs水平通过激活mTORC1途径导致糖尿病主动脉血管内皮损伤。PMPs显着降低了内皮糖萼面积以及glypican-1和occludin的表达水平(P <0.05)。有趣的是,猛禽siRNA和雷帕霉素可预防PMP诱导的内皮损伤。总之,增加的PMPs水平通过激活mTORC1途径导致糖尿病主动脉血管内皮损伤。
更新日期:2019-01-26
中文翻译:

血小板微粒通过mTORC1途径促成糖尿病的主动脉血管内皮损伤。
血小板微粒(PMP)与糖尿病大血管并发症密切相关。本研究旨在探讨糖尿病患者中PMPs对主动脉血管内皮损伤的影响并探讨其潜在机制。腹膜内注射链脲佐菌素可在体内产生糖尿病大鼠模型,体外使用经PMP处理的人脐静脉内皮细胞(HUVEC)。在链脲佐菌素诱导的糖尿病大鼠中,在第4、8和12周时,循环和主动脉组织中的PMP水平呈时间依赖性增加(P <0.05)。阿司匹林在每个时间点均显着抑制PMP水平(P <0.05)。在糖尿病大鼠中,内皮一氧化氮水平显着降低,同时内皮通透性增加。PMP被HUVEC内在化,并主要聚集在细胞核周围。PMP将内皮一氧化氮水平抑制到约50%,并导致活性氧的产生增加约两倍。此外,PMPs显着降低了内皮糖萼的面积以及glypican-1和occludin的表达水平(P <0.05)。有趣的是,猛禽siRNA和雷帕霉素可预防PMP诱导的内皮损伤。总之,增加的PMPs水平通过激活mTORC1途径导致糖尿病主动脉血管内皮损伤。PMPs显着降低了内皮糖萼面积以及glypican-1和occludin的表达水平(P <0.05)。有趣的是,猛禽siRNA和雷帕霉素可预防PMP诱导的内皮损伤。总之,增加的PMPs水平通过激活mTORC1途径导致糖尿病主动脉血管内皮损伤。PMPs显着降低了内皮糖萼面积以及glypican-1和occludin的表达水平(P <0.05)。有趣的是,猛禽siRNA和雷帕霉素可预防PMP诱导的内皮损伤。总之,增加的PMPs水平通过激活mTORC1途径导致糖尿病主动脉血管内皮损伤。











































 京公网安备 11010802027423号
京公网安备 11010802027423号