当前位置:
X-MOL 学术
›
JAMA Surg.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Palliative Care and End-of-Life Outcomes Following High-risk Surgery.
JAMA Surgery ( IF 15.7 ) Pub Date : 2020-01-02 , DOI: 10.1001/jamasurg.2019.5083 Maria Yefimova 1, 2 , Rebecca A Aslakson 3, 4 , Lingyao Yang 5 , Ariadna Garcia 5 , Derek Boothroyd 5 , Randall C Gale 1 , Karleen Giannitrapani 1, 6 , Arden M Morris 7 , Jason M Johanning 8, 9 , Scott Shreve 10 , Melissa W Wachterman 11, 12, 13 , Karl A Lorenz 1, 14
JAMA Surgery ( IF 15.7 ) Pub Date : 2020-01-02 , DOI: 10.1001/jamasurg.2019.5083 Maria Yefimova 1, 2 , Rebecca A Aslakson 3, 4 , Lingyao Yang 5 , Ariadna Garcia 5 , Derek Boothroyd 5 , Randall C Gale 1 , Karleen Giannitrapani 1, 6 , Arden M Morris 7 , Jason M Johanning 8, 9 , Scott Shreve 10 , Melissa W Wachterman 11, 12, 13 , Karl A Lorenz 1, 14
Affiliation
|
Importance
Palliative care has the potential to improve care for patients and families undergoing high-risk surgery.
Objective
To characterize the use of perioperative palliative care and its association with family-reported end-of-life experiences of patients who died within 90 days of a high-risk surgical operation.
Design, Setting, and Participants
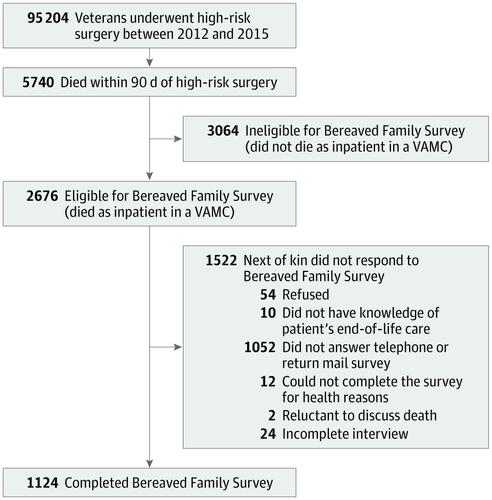
This secondary analysis of administrative data from a retrospective cross-sectional patient cohort was conducted in the Department of Veterans Affairs (VA) Healthcare System. Patients who underwent any of 227 high-risk operations between January 1, 2012, and December 31, 2015, were included.
Exposures
Palliative-care consultation within 30 days before or 90 days after surgery.
Main Outcomes and Measures
The outcomes were family-reported ratings of overall care, communication, and support in the patient's last month of life. The VA surveyed all families of inpatient decedents using the Bereaved Family Survey, a valid and reliable tool that measures patient and family-centered end-of-life outcomes.
Results
A total of 95 204 patients underwent high-risk operations in 129 inpatient VA Medical Centers. Most patients were 65 years or older (69 278 [72.8%]), and the most common procedures were cardiothoracic (31 157 [32.7%]) or vascular (23 517 [24.7%]). The 90-day mortality rate was 6.0% (5740 patients) and varied by surgical subspecialty (ranging from 278 of 7226 [3.8%] in urologic surgery to 875 of 6223 patients [14.1%] in neurosurgery). A multivariate mixed model revealed that families of decedents who received palliative care were 47% more likely to rate overall care in the last month of life as excellent than those who did not (odds ratio [OR], 1.47 [95% CI, 1.14-1.88]; P = .007), after adjusting for patient's characteristics, surgical subspecialty of the high-risk operation, and survey nonresponse. Similarly, families of decedents who received palliative care were more likely to rate end-of-life communication (OR, 1.43 [95% CI, 1.09-1.87]; P = .004) and support (OR, 1.31 [95% CI, 1.01-1.71]; P = .05) components of medical care as excellent. Of the entire cohort, 3374 patients (3.75%) had a palliative care consultation, and 770 patients (0.8%) received it before surgery. Of all decedents, 1632 (29.9%) had a palliative care consultation, with 319 (5.6%) receiving it before surgery.
Conclusions and Relevance
Receipt of a palliative consultation was associated with better ratings of overall end-of-life care, communication, and support, as reported by families of patients who died within 90 days of high-risk surgery. Yet only one-third of decedents was exposed to palliative care. Expanding integration of perioperative palliative care may benefit patients undergoing high-risk operations and their families.
中文翻译:

高风险手术后的姑息治疗和临终结果。
重要性姑息治疗具有改善对接受高风险手术的患者和家庭的护理的潜力。目的探讨围手术期姑息治疗的使用及其与高风险外科手术90天内死亡的患者家庭报告的临终经历的相关性。设计,设置和参与者对来自回顾性横断面患者队列的管理数据进行的二次分析是在退伍军人事务部(VA)的医疗保健系统中进行的。纳入在2012年1月1日至2015年12月31日期间进行过227次高风险手术的患者。暴露在手术前30天或手术后90天内进行姑息治疗咨询。主要结果和衡量指标结果是家庭报告的总体护理,沟通,和患者生命最后一个月的支持。弗吉尼亚州使用丧亲家庭调查(Bereaved Family Survey)对住院患者的所有家庭进行了调查,这是一种有效且可靠的工具,可以衡量以患者和家庭为中心的生命结局。结果在129个住院的VA医疗中心中,共有95 204名患者接受了高风险手术。大多数患者为65岁或以上(69 278 [72.8%]),最常见的手术是心胸(31 157 [32.7%])或血管(23 517 [24.7%])。90天死亡率为6.0%(5740例患者),具体因手术亚专业而异(泌尿外科手术的7226例中的278例[3.8%],神经外科手术的6222例中有875例[14.1%])。多元混合模型显示,接受姑息治疗的死者家属对生命最后一个月的总体治疗的评价比不接受姑息治疗的家庭的评价高47%(几率[OR]为1.47 [95%CI,1.14] [1.88]; P = .007),在针对患者的特征,高风险手术的外科专业进行调整后,对无反应进行调查。同样,接受姑息治疗的死者家属更有可能评价临终沟通(OR,1.43 [95%CI,1.09-1.87]; P = .004)和抚养费(OR,1.31 [95%CI, 1.01-1.71]; P = .05)极佳的医疗护理组件。在整个队列中,有3374例患者(3.75%)接受了姑息治疗咨询,而770例患者(0.8%)在手术前接受了姑息治疗。在所有死者中,有1632名(29.9%)接受姑息治疗咨询,其中319名(5。6%)在手术前接受。结论与相关性据高危手术90天内死亡的患者家属报告,姑息性咨询的收据与更好的总体临终护理,沟通和支持评级有关。然而,只有三分之一的死者曾接受过姑息治疗。围手术期姑息治疗的扩大整合可能会使正在进行高风险手术的患者及其家人受益。
更新日期:2020-02-19
中文翻译:

高风险手术后的姑息治疗和临终结果。
重要性姑息治疗具有改善对接受高风险手术的患者和家庭的护理的潜力。目的探讨围手术期姑息治疗的使用及其与高风险外科手术90天内死亡的患者家庭报告的临终经历的相关性。设计,设置和参与者对来自回顾性横断面患者队列的管理数据进行的二次分析是在退伍军人事务部(VA)的医疗保健系统中进行的。纳入在2012年1月1日至2015年12月31日期间进行过227次高风险手术的患者。暴露在手术前30天或手术后90天内进行姑息治疗咨询。主要结果和衡量指标结果是家庭报告的总体护理,沟通,和患者生命最后一个月的支持。弗吉尼亚州使用丧亲家庭调查(Bereaved Family Survey)对住院患者的所有家庭进行了调查,这是一种有效且可靠的工具,可以衡量以患者和家庭为中心的生命结局。结果在129个住院的VA医疗中心中,共有95 204名患者接受了高风险手术。大多数患者为65岁或以上(69 278 [72.8%]),最常见的手术是心胸(31 157 [32.7%])或血管(23 517 [24.7%])。90天死亡率为6.0%(5740例患者),具体因手术亚专业而异(泌尿外科手术的7226例中的278例[3.8%],神经外科手术的6222例中有875例[14.1%])。多元混合模型显示,接受姑息治疗的死者家属对生命最后一个月的总体治疗的评价比不接受姑息治疗的家庭的评价高47%(几率[OR]为1.47 [95%CI,1.14] [1.88]; P = .007),在针对患者的特征,高风险手术的外科专业进行调整后,对无反应进行调查。同样,接受姑息治疗的死者家属更有可能评价临终沟通(OR,1.43 [95%CI,1.09-1.87]; P = .004)和抚养费(OR,1.31 [95%CI, 1.01-1.71]; P = .05)极佳的医疗护理组件。在整个队列中,有3374例患者(3.75%)接受了姑息治疗咨询,而770例患者(0.8%)在手术前接受了姑息治疗。在所有死者中,有1632名(29.9%)接受姑息治疗咨询,其中319名(5。6%)在手术前接受。结论与相关性据高危手术90天内死亡的患者家属报告,姑息性咨询的收据与更好的总体临终护理,沟通和支持评级有关。然而,只有三分之一的死者曾接受过姑息治疗。围手术期姑息治疗的扩大整合可能会使正在进行高风险手术的患者及其家人受益。











































 京公网安备 11010802027423号
京公网安备 11010802027423号