Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association between gestational weight gain and severe adverse birth outcomes in Washington State, US: A population-based retrospective cohort study, 2004-2013.
PLOS Medicine ( IF 10.5 ) Pub Date : 2019-12-30 , DOI: 10.1371/journal.pmed.1003009 U Vivian Ukah 1 , Hamideh Bayrampour 2 , Yasser Sabr 3 , Neda Razaz 4 , Wee-Shian Chan 5 , Kenneth I Lim 6 , Sarka Lisonkova 6, 7
PLOS Medicine ( IF 10.5 ) Pub Date : 2019-12-30 , DOI: 10.1371/journal.pmed.1003009 U Vivian Ukah 1 , Hamideh Bayrampour 2 , Yasser Sabr 3 , Neda Razaz 4 , Wee-Shian Chan 5 , Kenneth I Lim 6 , Sarka Lisonkova 6, 7
Affiliation
|
BACKGROUND
Suboptimal weight gain during pregnancy is a potentially modifiable risk factor. We aimed to investigate the association between suboptimal gestational weight gain and severe adverse birth outcomes by pre-pregnancy body mass index (BMI) categories, including obesity class I to III.
METHODS AND FINDINGS
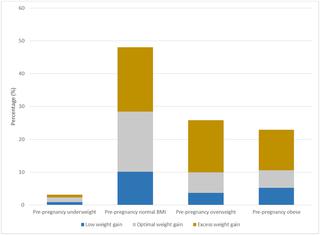
We conducted a population-based study of pregnant women with singleton hospital births in Washington State, US, between 2004 and 2013. Optimal, low, and excess weight gain in each BMI category was calculated based on weight gain by gestational age as recommended by the American College of Obstetricians and Gynecologists and the Institute of Medicine. Primary composite outcomes were (1) maternal death and/or severe maternal morbidity (SMM) and (2) perinatal death and/or severe neonatal morbidity. Logistic regression was used to obtain adjusted odds ratios (AORs) and 95% confidence intervals. Overall, 722,839 women with information on pre-pregnancy BMI were included. Of these, 3.1% of women were underweight, 48.1% had normal pre-pregnancy BMI, 25.8% were overweight, and 23.0% were obese. Only 31.5% of women achieved optimal gestational weight gain. Women who had low weight gain were more likely to be African American and have Medicaid health insurance, while women with excess weight gain were more likely to be non-Hispanic white and younger than women with optimal weight gain in each pre-pregnancy BMI category. Compared with women who had optimal weight gain, those with low gestational weight gain had a higher rate of maternal death, 7.97 versus 2.63 per 100,000 (p = 0.027). In addition, low weight gain was associated with the composite adverse maternal outcome (death/SMM) in women with normal pre-pregnancy BMI and in overweight women (AOR 1.12, 95% CI 1.04-1.21, p = 0.004, and AOR 1.17, 95% CI 1.04-1.32, p = 0.009, respectively) compared to women in the same pre-pregnancy BMI category who had optimal weight gain. Similarly, excess gestational weight gain was associated with increased rates of death/SMM among women with normal pre-pregnancy BMI (AOR 1.20, 95% CI 1.12-1.28, p < 0.001) and obese women (AOR 1.12, 95% CI 1.01-1.23, p = 0.019). Low gestational weight gain was associated with perinatal death and severe neonatal morbidity regardless of pre-pregnancy BMI, including obesity classes I, II, and III, while excess weight gain was associated with severe neonatal morbidity only in women who were underweight or had normal BMI prior to pregnancy. Study limitations include the ascertainment of pre-pregnancy BMI using self-report, and lack of data availability for the most recent years.
CONCLUSIONS
In this study, we found that most women do not achieve optimal weight gain during pregnancy. Low weight gain was associated with increased risk of severe adverse birth outcomes, and in particular with maternal death and perinatal death. Excess gestational weight gain was associated with severe adverse birth outcomes, except for women who were overweight prior to pregnancy. Weight gain recommendations for this group may need to be reassessed. It is important to counsel women during pregnancy about specific risks associated with both low and excess weight gain.
中文翻译:

美国华盛顿州妊娠体重增加与严重不良出生结局之间的关联:一项基于人群的回顾性队列研究,2004-2013年。
背景技术怀孕期间体重增加不理想是潜在的可改变的危险因素。我们旨在通过孕前体重指数(BMI)类别(包括I至III级肥胖)调查次佳妊娠体重增加与严重不良分娩结局之间的关系。方法和研究结果我们在2004年至2013年间对美国华盛顿州单身医院出生的孕妇进行了基于人群的研究。每种BMI类别的最佳,低和超重体重是根据胎龄增加的体重计算得出的。由美国妇产科学院和医学研究所推荐。主要的综合结局为(1)产妇死亡和/或严重的母亲发病率(SMM)和(2)围产期死亡和/或严重的新生儿发病率。使用Logistic回归获得调整的优势比(AOR)和95%的置信区间。总共纳入了722839名了解孕前BMI信息的妇女。其中,有3.1%的女性体重过轻,48.1%的孕前BMI正常,超重的25.8%和肥胖的23.0%。只有31.5%的女性达到了最佳的妊娠体重增长。在每个孕前BMI类别中,体重增加较低的女性更有可能是非裔美国人并拥有医疗补助医疗保险,而体重增加过多的女性则比那些体重增加最佳的女性更容易成为非西班牙裔白人和年轻女性。与体重增加最佳的女性相比,妊娠体重增加低的女性孕产妇死亡率更高,分别为7.97比2.100,000 / 10万(p = 0.027)。此外,低体重增加与孕前BMI正常的女性和超重女性的复合不良母体结局(死亡/ SMM)相关(AOR 1.12,95%CI 1.04-1.21,p = 0.004,AOR 1.17,95%CI与相同的孕前BMI类别中具有最佳体重增加的女性相比,分别为1.04-1.32,p = 0.009)。同样,孕前体重指数正常的女性(AOR 1.20,95%CI 1.12-1.28,p <0.001)和肥胖的女性(AOR 1.12,95%CI 1.01)中,妊娠期体重增加过多与死亡率/ SMM的增加相关。 1.23,p = 0.019)。低妊娠体重增加与围产期死亡和严重的新生儿发病率相关,而与孕前BMI无关,包括肥胖症I,II和III级,而仅在体重不足或妊娠前BMI正常的女性中,体重增加过重才与严重的新生儿发病率相关。研究的局限性包括使用自我报告确定怀孕前的BMI,以及最近几年缺乏数据可用性。结论在这项研究中,我们发现大多数女性在怀孕期间未达到最佳体重增加。体重增加低与严重不良分娩结果的风险增加有关,特别是与孕产妇死亡和围产期死亡有关。妊娠期体重增加过多与严重的不良出生结局有关,但怀孕前超重的妇女除外。对于该组的体重增加建议可能需要重新评估。
更新日期:2020-01-14
中文翻译:

美国华盛顿州妊娠体重增加与严重不良出生结局之间的关联:一项基于人群的回顾性队列研究,2004-2013年。
背景技术怀孕期间体重增加不理想是潜在的可改变的危险因素。我们旨在通过孕前体重指数(BMI)类别(包括I至III级肥胖)调查次佳妊娠体重增加与严重不良分娩结局之间的关系。方法和研究结果我们在2004年至2013年间对美国华盛顿州单身医院出生的孕妇进行了基于人群的研究。每种BMI类别的最佳,低和超重体重是根据胎龄增加的体重计算得出的。由美国妇产科学院和医学研究所推荐。主要的综合结局为(1)产妇死亡和/或严重的母亲发病率(SMM)和(2)围产期死亡和/或严重的新生儿发病率。使用Logistic回归获得调整的优势比(AOR)和95%的置信区间。总共纳入了722839名了解孕前BMI信息的妇女。其中,有3.1%的女性体重过轻,48.1%的孕前BMI正常,超重的25.8%和肥胖的23.0%。只有31.5%的女性达到了最佳的妊娠体重增长。在每个孕前BMI类别中,体重增加较低的女性更有可能是非裔美国人并拥有医疗补助医疗保险,而体重增加过多的女性则比那些体重增加最佳的女性更容易成为非西班牙裔白人和年轻女性。与体重增加最佳的女性相比,妊娠体重增加低的女性孕产妇死亡率更高,分别为7.97比2.100,000 / 10万(p = 0.027)。此外,低体重增加与孕前BMI正常的女性和超重女性的复合不良母体结局(死亡/ SMM)相关(AOR 1.12,95%CI 1.04-1.21,p = 0.004,AOR 1.17,95%CI与相同的孕前BMI类别中具有最佳体重增加的女性相比,分别为1.04-1.32,p = 0.009)。同样,孕前体重指数正常的女性(AOR 1.20,95%CI 1.12-1.28,p <0.001)和肥胖的女性(AOR 1.12,95%CI 1.01)中,妊娠期体重增加过多与死亡率/ SMM的增加相关。 1.23,p = 0.019)。低妊娠体重增加与围产期死亡和严重的新生儿发病率相关,而与孕前BMI无关,包括肥胖症I,II和III级,而仅在体重不足或妊娠前BMI正常的女性中,体重增加过重才与严重的新生儿发病率相关。研究的局限性包括使用自我报告确定怀孕前的BMI,以及最近几年缺乏数据可用性。结论在这项研究中,我们发现大多数女性在怀孕期间未达到最佳体重增加。体重增加低与严重不良分娩结果的风险增加有关,特别是与孕产妇死亡和围产期死亡有关。妊娠期体重增加过多与严重的不良出生结局有关,但怀孕前超重的妇女除外。对于该组的体重增加建议可能需要重新评估。











































 京公网安备 11010802027423号
京公网安备 11010802027423号