当前位置:
X-MOL 学术
›
JAMA Neurol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Prognostic Value of Spreading Depolarizations in Patients With Severe Traumatic Brain Injury.
JAMA Neurology ( IF 20.4 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamaneurol.2019.4476 Jed A Hartings 1, 2 , Norberto Andaluz 1, 3 , M Ross Bullock 4 , Jason M Hinzman 1 , Bruce Mathern 5 , Clemens Pahl 6 , Ava Puccio 7 , Lori A Shutter 1, 8 , Anthony J Strong 9 , Achala Vagal 10 , J Adam Wilson 1 , Jens P Dreier 11 , Laura B Ngwenya 1, 2 , Brandon Foreman 1, 2 , Laura Pahren 12 , Hester Lingsma 13 , David O Okonkwo 7
JAMA Neurology ( IF 20.4 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamaneurol.2019.4476 Jed A Hartings 1, 2 , Norberto Andaluz 1, 3 , M Ross Bullock 4 , Jason M Hinzman 1 , Bruce Mathern 5 , Clemens Pahl 6 , Ava Puccio 7 , Lori A Shutter 1, 8 , Anthony J Strong 9 , Achala Vagal 10 , J Adam Wilson 1 , Jens P Dreier 11 , Laura B Ngwenya 1, 2 , Brandon Foreman 1, 2 , Laura Pahren 12 , Hester Lingsma 13 , David O Okonkwo 7
Affiliation
|
Importance
Advances in treatment of traumatic brain injury are hindered by the inability to monitor pathological mechanisms in individual patients for targeted neuroprotective treatment. Spreading depolarizations, a mechanism of lesion development in animal models, are a novel candidate for clinical monitoring in patients with brain trauma who need surgery.
Objective
To test the null hypothesis that spreading depolarizations are not associated with worse neurologic outcomes.
Design, Setting, and Participants
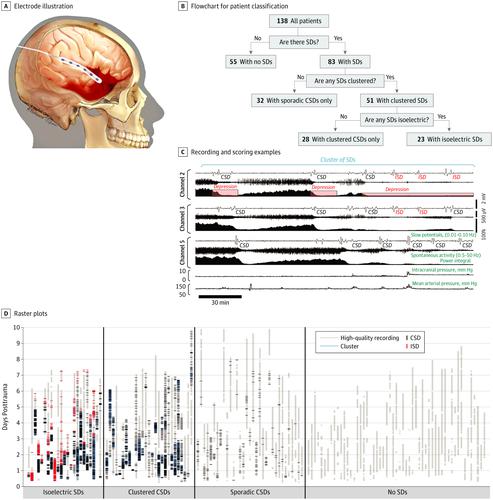
This prospective, observational, multicenter cohort study was conducted from February 2009 to August 2013 in 5 level 1 trauma centers. Consecutive patients who required neurological surgery for treatment of acute brain trauma and for whom research consent could be obtained were enrolled; participants were excluded because of technical problems in data quality, patient withdrawal, or loss to follow-up. Primary statistical analysis took place from April to December 2018. Evaluators of outcome assessments were blinded to other measures.
Interventions
A 6-contact electrode strip was placed on the brain surface during surgery for continuous electrocorticography during intensive care.
Main Outcomes and Measures
Electrocorticography was scored for depolarizations, following international consensus procedures. Six-month outcomes were assessed by the Glasgow Outcome Scale-Extended score.
Results
A total of 157 patients were initially enrolled; 19 were subsequently excluded. The 138 remaining patients (104 men [75%]; median [interquartile range] age, 45 [29-64] years) underwent a median (interquartile range) of 75.5 (42.2-117.1) hours of electrocorticography. A total of 2837 spreading depolarizations occurred in 83 of 138 patients (60.1% incidence) who, compared with patients who did not have spreading depolarizations, had lower prehospital systolic blood pressure levels (mean [SD], 133 [31] mm Hg vs 146 [33] mm Hg; P = .03), more traumatic subarachnoid hemorrhage (depolarization incidences of 17 of 37 [46%], 18 of 32 [56%], 22 of 33 [67%], and 23 of 30 patients [77%] for Morris-Marshall Grades 0, 1, 2, and 3/4, respectively; P = .047), and worse radiographic pathology (in 38 of 73 patients [52%] and 42 of 60 patients [70%] for Rotterdam Scores 2-4 vs 5-6, respectively; P = .04). Of patients with depolarizations, 32 of 83 (39%) had only sporadic events that induced cortical spreading depression of spontaneous electrical activity, whereas 51 of 83 patients (61%) exhibited temporal clusters of depolarizations (≥3 in a 2-hour span). Nearly half of those with clusters (23 of 51 [45%]) also had depolarizations in an electrically silent area of the cortex (isoelectric spreading depolarization). Patients with clusters did not improve in motor neurologic examinations from presurgery to postelectrocorticography, while other patients did improve. In multivariate ordinal regression adjusting for baseline prognostic variables, the occurrence of depolarization clusters had an odds ratio of 2.29 (95% CI, 1.13-4.65; P = .02) for worse outcomes.
Conclusions and Relevance
In this cohort study of patients with acute brain trauma, spreading depolarizations were predominant but heterogeneous and independently associated with poor neurologic recovery. Monitoring the occurrence of spreading depolarizations may identify patients most likely to benefit from targeted management strategies.
中文翻译:

扩展去极化对严重颅脑外伤患者的预后价值。
重要性由于无法监测个别患者的靶向神经保护性治疗的病理机制,因此阻碍了创伤性脑损伤的治疗进展。扩散性去极化是动物模型中病变发展的一种机制,是需要手术治疗的脑外伤患者临床监测的新选择。目的检验零假设,即去极化扩展与神经功能恶化无关。设计,设置和参与者这项前瞻性,观察性,多中心队列研究于2009年2月至2013年8月在5个1级创伤中心进行。入组需要神经外科手术治疗急性脑外伤并获得研究同意的连续患者;由于数据质量,患者退出或随访失败等技术问题而将参与者排除在外。初步统计分析于2018年4月至12月进行。结果评估的评估者对其他措施不知情。干预措施在手术过程中,将6触点电极条放置在脑表面上,以便在重症监护期间进行连续皮层造影。主要结果和措施按照国际共识的程序,对皮层照相术的去极化进行评分。通过格拉斯哥结局量表-扩展分数评估六个月的结局。结果最初纳入157例患者。随后排除了19个。其余138名患者(104名男性[75%];中位[四分位间距]年龄为45 [29-64]岁)的中位值(四分位间距)为75.5(42.2-117)。1)皮质脑电图的小时数。138例患者中,有83例发生了2837例扩散性去极化,与未扩散性去极化的患者相比,院前收缩压水平较低(平均[SD],133 [31] mm Hg vs 146) [33]毫米汞柱; P = .03),更多的创伤性蛛网膜下腔出血(去极化发生率:37 [17] [46%],18 [32] [56%],22 [33] [67%]和30 30例[23] [ [77%]的Morris-Marshall分别为0、1、2和3/4级; P = .047),并且放射学病理学恶化(73例患者中的38例[52%]和60例患者中的42例[70%])分别为鹿特丹2-4分和5-6分; P = .04)。在去极化患者中,只有83名患者中有32名(39%)偶发事件导致自发性电活动的皮质扩散抑制,而83例患者中有51例(61%)表现出暂时性的去极化簇(在2小时内≥3)。具有簇的那些中的近一半(51个中的23个[45%])在皮质的电性静默区域也具有去极化作用(等电扩展去极化作用)。从手术前到脑电图检查,簇状患者的运动神经系统检查无改善,而其他患者则有改善。在针对基线预后变量进行调整的多元有序回归中,去极化簇的发生率比结果为2.29(95%CI,1.13-4.65; P = .02)。结论与相关性在这项针对急性脑外伤患者的队列研究中,扩散性去极化是主要的但异质性的,并且独立于不良的神经功能恢复。
更新日期:2020-04-01
中文翻译:

扩展去极化对严重颅脑外伤患者的预后价值。
重要性由于无法监测个别患者的靶向神经保护性治疗的病理机制,因此阻碍了创伤性脑损伤的治疗进展。扩散性去极化是动物模型中病变发展的一种机制,是需要手术治疗的脑外伤患者临床监测的新选择。目的检验零假设,即去极化扩展与神经功能恶化无关。设计,设置和参与者这项前瞻性,观察性,多中心队列研究于2009年2月至2013年8月在5个1级创伤中心进行。入组需要神经外科手术治疗急性脑外伤并获得研究同意的连续患者;由于数据质量,患者退出或随访失败等技术问题而将参与者排除在外。初步统计分析于2018年4月至12月进行。结果评估的评估者对其他措施不知情。干预措施在手术过程中,将6触点电极条放置在脑表面上,以便在重症监护期间进行连续皮层造影。主要结果和措施按照国际共识的程序,对皮层照相术的去极化进行评分。通过格拉斯哥结局量表-扩展分数评估六个月的结局。结果最初纳入157例患者。随后排除了19个。其余138名患者(104名男性[75%];中位[四分位间距]年龄为45 [29-64]岁)的中位值(四分位间距)为75.5(42.2-117)。1)皮质脑电图的小时数。138例患者中,有83例发生了2837例扩散性去极化,与未扩散性去极化的患者相比,院前收缩压水平较低(平均[SD],133 [31] mm Hg vs 146) [33]毫米汞柱; P = .03),更多的创伤性蛛网膜下腔出血(去极化发生率:37 [17] [46%],18 [32] [56%],22 [33] [67%]和30 30例[23] [ [77%]的Morris-Marshall分别为0、1、2和3/4级; P = .047),并且放射学病理学恶化(73例患者中的38例[52%]和60例患者中的42例[70%])分别为鹿特丹2-4分和5-6分; P = .04)。在去极化患者中,只有83名患者中有32名(39%)偶发事件导致自发性电活动的皮质扩散抑制,而83例患者中有51例(61%)表现出暂时性的去极化簇(在2小时内≥3)。具有簇的那些中的近一半(51个中的23个[45%])在皮质的电性静默区域也具有去极化作用(等电扩展去极化作用)。从手术前到脑电图检查,簇状患者的运动神经系统检查无改善,而其他患者则有改善。在针对基线预后变量进行调整的多元有序回归中,去极化簇的发生率比结果为2.29(95%CI,1.13-4.65; P = .02)。结论与相关性在这项针对急性脑外伤患者的队列研究中,扩散性去极化是主要的但异质性的,并且独立于不良的神经功能恢复。











































 京公网安备 11010802027423号
京公网安备 11010802027423号