当前位置:
X-MOL 学术
›
Lancet Diabetes Endocrinol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of insulin resistance and β-cell dysfunction with incident diabetes among adults in China: a nationwide, population-based, prospective cohort study.
The Lancet Diabetes & Endocrinology ( IF 44.0 ) Pub Date : 2019-12-23 , DOI: 10.1016/s2213-8587(19)30425-5 Tiange Wang 1 , Jieli Lu 1 , Lixin Shi 2 , Gang Chen 3 , Min Xu 1 , Yu Xu 1 , Qing Su 4 , Yiming Mu 5 , Lulu Chen 6 , Ruying Hu 7 , Xulei Tang 8 , Xuefeng Yu 9 , Mian Li 1 , Zhiyun Zhao 1 , Yuhong Chen 1 , Li Yan 10 , Guijun Qin 11 , Qin Wan 12 , Meng Dai 1 , Di Zhang 1 , Zhengnan Gao 13 , Guixia Wang 14 , Feixia Shen 15 , Zuojie Luo 16 , Yingfen Qin 16 , Li Chen 17 , Yanan Huo 18 , Qiang Li 19 , Zhen Ye 7 , Yinfei Zhang 20 , Chao Liu 21 , Youmin Wang 22 , Shengli Wu 23 , Tao Yang 24 , Huacong Deng 25 , Jiajun Zhao 26 , Shenghan Lai 27 , Yufang Bi 1 , Ralph A DeFronzo 28 , Weiqing Wang 1 , Guang Ning 1 ,
The Lancet Diabetes & Endocrinology ( IF 44.0 ) Pub Date : 2019-12-23 , DOI: 10.1016/s2213-8587(19)30425-5 Tiange Wang 1 , Jieli Lu 1 , Lixin Shi 2 , Gang Chen 3 , Min Xu 1 , Yu Xu 1 , Qing Su 4 , Yiming Mu 5 , Lulu Chen 6 , Ruying Hu 7 , Xulei Tang 8 , Xuefeng Yu 9 , Mian Li 1 , Zhiyun Zhao 1 , Yuhong Chen 1 , Li Yan 10 , Guijun Qin 11 , Qin Wan 12 , Meng Dai 1 , Di Zhang 1 , Zhengnan Gao 13 , Guixia Wang 14 , Feixia Shen 15 , Zuojie Luo 16 , Yingfen Qin 16 , Li Chen 17 , Yanan Huo 18 , Qiang Li 19 , Zhen Ye 7 , Yinfei Zhang 20 , Chao Liu 21 , Youmin Wang 22 , Shengli Wu 23 , Tao Yang 24 , Huacong Deng 25 , Jiajun Zhao 26 , Shenghan Lai 27 , Yufang Bi 1 , Ralph A DeFronzo 28 , Weiqing Wang 1 , Guang Ning 1 ,
Affiliation
|
BACKGROUND
National investigations on the interaction of insulin resistance, β-cell dysfunction, and obesity with the development of diabetes are scarce in China. We aimed to investigate the individual and joint associations of insulin resistance and β-cell dysfunction with incident diabetes, and to examine the modifying effect of BMI and waist circumference on these associations among adults with normal glucose tolerance and with prediabetes.
METHODS
In this nationwide, population-based, prospective cohort study, we analysed data from the China Cardiometabolic Disease and Cancer Cohort Study, which recruited adults aged 40 years or older during 2011-12 (baseline) and invited participants to attend follow-up visits in 2014-16. Patients with diabetes at baseline, missing data for baseline measures of glucose tolerance status, missing data for baseline homoeostasis model assessment (HOMA) indexes, missing data for baseline covariates, and missing data for measures of glucose tolerance status at follow-up visits were excluded. At baseline and follow-up visits, a comprehensive set of questionnaires, clinical measurements, oral glucose tolerance tests, and laboratory examinations were carried out following standardised protocols. Glucose tolerance status and prediabetes were defined according to the American Diabetes Association 2010 criteria. In the main analysis, we examined the contributions of insulin resistance (HOMA of insulin resistance [HOMA-IR]) and β-cell dysfunction (HOMA of β-cell function [HOMA-B]) to diabetes risk, and evaluated the impact of obesity on these associations.
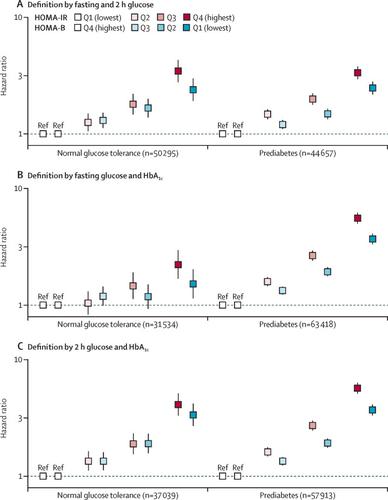
FINDINGS
94 952 participants (31 517 men and 63 435 women) were included in the analysis. High HOMA-IR was associated with a greater hazard of diabetes (quartile 4 vs 1: hazard ratio [HR] 6·70, 95% CI 6·08-7·39; per unit increase in Z score: HR 2·17, 95% CI 2·10-2·24) than low HOMA-B (quartile 1 vs 4: 4·08, 3·72-4·48; per unit decrease in Z score: 1·92, 1·85-2·00). Approximately 24·4% (95% CI 23·6-25·2) of the incident diabetes could be attributed to insulin resistance and 12·4% (11·2-13·7) could be attributed to β-cell dysfunction. The HRs for diabetes were 1·83 (95% CI 1·72-1·95) per unit increase in Z score of HOMA-IR and 2·03 (1·86-2·21) per unit decrease in Z score of HOMA-B among participants with normal weight; the corresponding HRs for diabetes were 2·02 (1·93-2·11) and 1·88 (1·79-1·98) among participants with obesity (pinteraction=0·0091). These associations and interactions were similar for participants with normal glucose tolerance or prediabetes.
INTERPRETATION
Insulin resistance shows a stronger association with incident diabetes than does β-cell dysfunction in Chinese adults, and this association pattern was more prominent among adults with obesity. Given the limitations of HOMA indexes as surrogate measures of insulin resistance and β-cell dysfunction, these findings should be interpreted with caution.
FUNDING
National Natural Science Foundation of China.
更新日期:2020-01-22











































 京公网安备 11010802027423号
京公网安备 11010802027423号