The Lancet HIV ( IF 12.8 ) Pub Date : 2019-12-20 , DOI: 10.1016/s2352-3018(19)30339-x Kunjal Patel 1 , Brad Karalius 2 , Kathleen Powis 3 , Deborah Kacanek 4 , Claire Berman 2 , Anna-Barbara Moscicki 5 , Mary Paul 6 , Katherine Tassiopoulos 1 , George R Seage 2 ,
|
Background
Small studies reported poor post-partum outcomes among young women living with perinatal HIV infection who are now ageing into adulthood and becoming pregnant. For targeted clinical intervention, we sought to identify women in this population at risk of poor post-partum virological control.
Methods
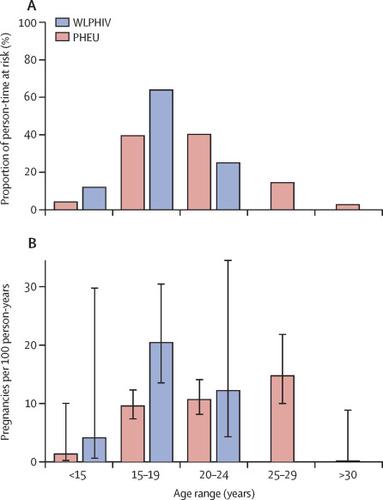
We abstracted data on pregnancy history for women living with perinatal HIV infection in the Pediatric HIV/AIDS Cohort Study-AMP Up protocol, a prospective study of young adults living with perinatal HIV from 14 sites in the USA. Linear models with generalised estimating equations described trends in HIV viral load through 1 year post-pregnancy by pregnancy outcome. We used group-based trajectory modelling to identify viral load trajectory groups in the first post-partum year after livebirths. We then compared sociodemographic and clinical factors across identified groups. We defined viraemia as 400 copies per mL or more.
Findings
Between April 15, 2014, and Oct 1, 2017, we enrolled 323 women, of whom 234 had perinatal HIV infection, and reported age at sexual debut and history of heterosexual vaginal intercourse. Of the 172 pregnancies recorded in these women, 147 (85%, 104 livebirths and 43 spontaneous or elective abortions) were eligible for post-pregnancy viral load trajectory analyses (ie, had at least two viral loads in the year after end of pregnancy). Viral load increased by 0·7 log10 copies per mL (95% CI 0·5 to 1·0) in the first 12 weeks post partum after 104 livebirths, and subsequently stabilised from 13 weeks to 1 year post partum (slope −0·01 log10 copies per mL, 95% CI −0·3 to 0·3). By comparison, the average viral load trajectory after 43 spontaneous or elective abortions remained at less than 400 copies per mL. We identified three distinct groups of viral load trajectories after 104 livebirths, classified as reflecting sustained suppression (31 [30%]), rebound viraemia (55 [53%]), and persistent viraemia (18 [17%]). Women with sustained post-partum suppression were older at conception (22·9 years, IQR 19·4–25·9) than those with rebound viraemia (20·4 years, 18·8–22·2), or persistent post-partum viraemia (19·0 years, 17·7–20·5). Pre-conception viraemia and immune suppression were also strong risk factors for post-partum viraemia.
Interpretation
Despite success achieving viral load suppression during pregnancy, women living with perinatal HIV infection have a high risk of post-partum viraemia. Younger age at conception, pre-conception viraemia, and pre-conception immune suppression could identify women in this population most likely to benefit from post-partum adherence interventions.
Funding
National Institutes of Health.
中文翻译:

美国围产期HIV感染妇女产后病毒载量的趋势:一项前瞻性队列研究。
背景
小型研究报告说,患有围产期艾滋病毒感染的年轻妇女的产后结局较差,这些妇女现已成年并怀孕。为了进行有针对性的临床干预,我们试图确定该人群中有产后病毒学控制不良风险的妇女。
方法
我们在“小儿HIV / AIDS队列研究-AMP Up”方案中提取了围生期HIV感染妇女的妊娠史数据,这项前瞻性研究来自美国14个地方,对围生期HIV感染的年轻成年人进行前瞻性研究。具有广义估计方程的线性模型通过怀孕结局描述了怀孕后1年内HIV病毒载量的趋势。我们使用基于组的轨迹模型来确定出生后产后第一年的病毒载量轨迹组。然后,我们比较了确定人群中的社会人口统计学和临床因素。我们将病毒血症定义为每毫升400拷贝或更多。
发现
在2014年4月15日至2017年10月1日之间,我们招募了323名女性,其中234名感染了围生期HIV,并报告了初次性交年龄和异性阴道交往史。在这些妇女记录的172例怀孕中,有147例(85%,104例分娩和43例自然流产或选择性流产)有资格进行孕后病毒载量轨迹分析(即,在妊娠结束后的第二年中至少有两次病毒载量) 。在分娩104次后的最初12周,病毒载量每毫升增加0·7 log 10份(95%CI 0·5至1·0),随后在分娩后13周至1年稳定(斜率−0 ·01日志10每毫升副本数,95%CI -0·3至0·3)。相比之下,43次自然流产或选择性流产后的平均病毒载量轨迹仍低于每毫升400个拷贝。我们确定了104个分娩后的三组不同的病毒载量轨迹,分为持续抑制(31 [30%]),反弹性病毒血症(55 [53%])和持续性病毒血症(18 [17%])。持续产后抑制的妇女在受孕时(22·9岁,IQR 19·4-25·9)比反弹性病毒血症(20·4岁,18·8-22·2)或持续性产后高。局部病毒血症(19·0岁,17·7-20·5)。孕前病毒血症和免疫抑制也是产后病毒血症的重要危险因素。
解释
尽管成功地抑制了怀孕期间的病毒载量,但围产期感染HIV的妇女产后病毒血症的风险很高。受孕年龄较小,受孕前病毒血症和受孕前免疫抑制可以确定该人群中的女性最有可能从产后依从性干预中受益。
资金
国立卫生研究院。











































 京公网安备 11010802027423号
京公网安备 11010802027423号