Theranostics ( IF 12.4 ) Pub Date : 2020-01-01 , DOI: 10.7150/thno.40908 Dallan McMahon 1, 2 , Wendy Oakden 1 , Kullervo Hynynen 1, 2, 3
|
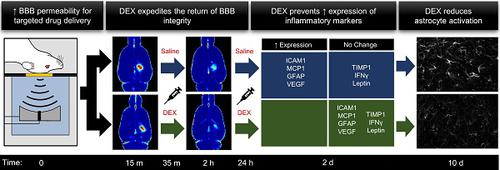
Rationale: Clinical trials are currently underway to test the safety and efficacy of delivering therapeutic agents across the blood-brain barrier (BBB) using focused ultrasound and microbubbles (FUS+MBs). While acoustic feedback control strategies have largely minimized the risk of overt tissue damage, transient induction of inflammatory processes have been observed following sonication in preclinical studies. The goal of this work was to explore the potential of post-sonication dexamethasone (DEX) administration as a means to mitigate treatment risk. Vascular permeability, inflammatory protein expression, blood vessel growth, and astrocyte activation were assessed.
Methods: A single-element focused transducer (transmit frequency = 580 kHz) and DefinityTM microbubbles were used to increase BBB permeability unilaterally in the dorsal hippocampi of adult male rats. Sonicating pressure was calibrated based on ultraharmonic emissions. Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) was used to quantitatively assess BBB permeability at 15 min (baseline) and 2 hrs following sonication. DEX was administered following baseline imaging and at 24 hrs post-FUS+MB exposure. Expression of key inflammatory proteins were assessed at 2 days, and astrocyte activation and blood vessel growth were assessed at 10 days post-FUS+MB exposure.
Results: Compared to saline-treated control animals, DEX administration expedited the restoration of BBB integrity at 2 hrs, and significantly limited the production of key inflammation-related proteins at 2 days, following sonication. Indications of FUS+MB-induced astrocyte activation and vascular growth were diminished at 10 days in DEX-treated animals, compared to controls.
Conclusions: These results suggest that DEX provides a means of modulating the duration of BBB permeability enhancement and may reduce the risk of inflammation-induced tissue damage, increasing the safety profile of this drug-delivery strategy. This effect may be especially relevant in scenarios for which the goal of treatment is to restore or preserve neural function and multiple sonications are required.
中文翻译:

研究地塞米松对聚焦超声和微泡暴露后血脑屏障通透性和炎症反应的影响。
理由:目前正在进行临床试验,以测试使用聚焦超声和微泡 (FUS+MBs) 跨越血脑屏障 (BBB) 递送治疗剂的安全性和有效性。虽然声反馈控制策略在很大程度上降低了明显组织损伤的风险,但在临床前研究中观察到超声处理后炎症过程的瞬时诱导。这项工作的目的是探索超声后地塞米松 (DEX) 给药作为降低治疗风险的一种手段的潜力。评估了血管通透性、炎症蛋白表达、血管生长和星形胶质细胞活化。
方法:使用单晶聚焦传感器(发射频率 = 580 kHz)和 Definity TM微泡单侧增加成年雄性大鼠背侧海马的 BBB 通透性。基于超谐波发射校准超声压力。动态对比增强磁共振成像 (DCE-MRI) 用于定量评估超声处理后 15 分钟(基线)和 2 小时的 BBB 通透性。在基线成像后和 FUS+MB 暴露后 24 小时施用 DEX。在 2 天评估关键炎症蛋白的表达,在 FUS+MB 暴露后 10 天评估星形胶质细胞活化和血管生长。
结果:与盐水处理的对照动物相比,DEX 给药在 2 小时内加速了 BBB 完整性的恢复,并在超声处理后 2 天显着限制了关键炎症相关蛋白的产生。与对照组相比,在 DEX 处理的动物中,FUS+MB 诱导的星形胶质细胞活化和血管生长的迹象在 10 天时减少。
结论:这些结果表明,DEX 提供了一种调节 BBB 通透性增强持续时间的方法,并可能降低炎症引起的组织损伤的风险,从而提高这种给药策略的安全性。在治疗目标是恢复或保留神经功能并且需要多次超声处理的情况下,这种效果可能特别相关。











































 京公网安备 11010802027423号
京公网安备 11010802027423号