Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of Transcarotid Artery Revascularization vs Transfemoral Carotid Artery Stenting With Stroke or Death Among Patients With Carotid Artery Stenosis
JAMA ( IF 63.1 ) Pub Date : 2019-12-17 , DOI: 10.1001/jama.2019.18441 Marc L Schermerhorn 1 , Patric Liang 1 , Jens Eldrup-Jorgensen 2 , Jack L Cronenwett 3 , Brian W Nolan 2 , Vikram S Kashyap 4 , Grace J Wang 5 , Raghu L Motaganahalli 6 , Mahmoud B Malas 7
JAMA ( IF 63.1 ) Pub Date : 2019-12-17 , DOI: 10.1001/jama.2019.18441 Marc L Schermerhorn 1 , Patric Liang 1 , Jens Eldrup-Jorgensen 2 , Jack L Cronenwett 3 , Brian W Nolan 2 , Vikram S Kashyap 4 , Grace J Wang 5 , Raghu L Motaganahalli 6 , Mahmoud B Malas 7
Affiliation
|
Importance
Several trials have observed higher rates of perioperative stroke following transfemoral carotid artery stenting compared with carotid endarterectomy. Transcarotid artery revascularization with flow reversal was recently introduced for carotid stenting. This technique was developed to decrease stroke risk seen with the transfemoral approach; however, its outcomes, compared with transfemoral carotid artery stenting, are not well characterized. Objective
To compare outcomes associated with transcarotid artery revascularization and transfemoral carotid artery stenting. Design, Setting, and Participants
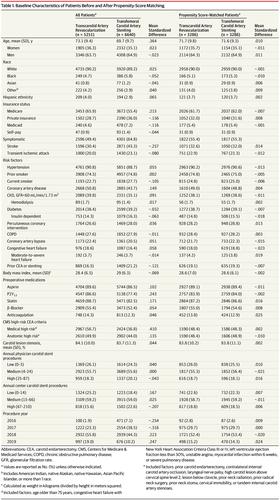
Exploratory propensity score-matched analysis of prospectively collected data from the Vascular Quality Initiative Transcarotid Artery Surveillance Project and Carotid Stent Registry of asymptomatic and symptomatic patients in the United States and Canada undergoing transcarotid artery revascularization and transfemoral carotid artery stenting for carotid artery stenosis, from September 2016 to April 2019. The final date for follow-up was May 29, 2019. Exposures
Transcarotid artery revascularization vs transfemoral carotid artery stenting. Main Outcomes and Measures
Outcomes included a composite end point of in-hospital stroke or death, stroke, death, myocardial infarction, as well as ipsilateral stroke or death at 1 year. In-hospital stroke was defined as ipsilateral or contralateral, cortical or vertebrobasilar, and ischemic or hemorrhagic stroke. Death was all-cause mortality. Results
During the study period, 5251 patients underwent transcarotid artery revascularization and 6640 patients underwent transfemoral carotid artery stenting. After matching, 3286 pairs of patients who underwent transcarotid artery revascularization or transfemoral carotid artery stenting were identified (transcarotid approach: mean [SD] age, 71.7 [9.8] years; 35.7% women; transfemoral approach: mean [SD] age, 71.6 [9.3] years; 35.1% women). Transcarotid artery revascularization was associated with a lower risk of in-hospital stroke or death (1.6% vs 3.1%; absolute difference, -1.52% [95% CI, -2.29% to -0.75%]; relative risk [RR], 0.51 [95% CI, 0.37 to 0.72]; P < .001), stroke (1.3% vs 2.4%; absolute difference, -1.10% [95% CI, -1.79% to -0.41%]; RR, 0.54 [95% CI, 0.38 to 0.79]; P = .001), and death (0.4% vs 1.0%; absolute difference, -0.55% [95% CI, -0.98% to -0.11%]; RR, 0.44 [95% CI, 0.23 to 0.82]; P = .008). There was no statistically significant difference in the risk of perioperative myocardial infarction between the 2 cohorts (0.2% for transcarotid vs 0.3% for the transfemoral approach; absolute difference, -0.09% [95% CI, -0.37% to 0.19%]; RR, 0.70 [95% CI, 0.27 to 1.84]; P = .47). At 1 year using Kaplan-Meier life-table estimation, the transcarotid approach was associated with a lower risk of ipsilateral stroke or death (5.1% vs 9.6%; hazard ratio, 0.52 [95% CI, 0.41 to 0.66]; P < .001). Transcarotid artery revascularization was associated with higher risk of access site complication resulting in interventional treatment (1.3% vs 0.8%; absolute difference, 0.52% [95% CI, -0.01% to 1.04%]; RR, 1.63 [95% CI, 1.02 to 2.61]; P = .04), whereas transfemoral carotid artery stenting was associated with more radiation (median fluoroscopy time, 5 minutes [interquartile range {IQR}, 3 to 7] vs 16 minutes [IQR, 11 to 23]; P < .001) and more contrast (median contrast used, 30 mL [IQR, 20 to 45] vs 80 mL [IQR, 55 to 122]; P < .001). Conclusions and Relevance
Among patients undergoing treatment for carotid stenosis, transcarotid artery revascularization, compared with transfemoral carotid artery stenting, was significantly associated with a lower risk of stroke or death.
中文翻译:

经颈动脉血运重建与经股颈动脉支架置入术与颈动脉狭窄患者中风或死亡的关系
重要性 多项试验观察到,与颈动脉内膜切除术相比,经股颈动脉支架置入术围手术期卒中的发生率更高。最近引入了具有血流逆转的经颈动脉血运重建术用于颈动脉支架置入术。这项技术的开发是为了降低经股动脉入路的中风风险;然而,与经股颈动脉支架置入术相比,其结果尚不明确。目的 比较经颈动脉血运重建术和经股颈动脉支架置入术的相关结果。设计、设置和参与者 对美国和加拿大接受经颈动脉血运重建和经股颈动脉支架植入术的血管质量倡议经颈动脉监测项目和颈动脉支架登记处前瞻性收集的数据进行探索性倾向评分匹配分析。颈动脉狭窄,从2016年9月到2019年4月。最终随访日期是2019年5月29日。暴露经颈动脉血运重建与经股颈动脉支架置入术。主要结局和措施 结局包括院内卒中或死亡、卒中、死亡、心肌梗塞以及一年内同侧卒中或死亡的复合终点。院内卒中被定义为同侧或对侧、皮质或椎基底动脉、缺血性或出血性卒中。死亡是全因死亡率。结果 研究期间,5251 名患者接受了经颈动脉血运重建术,6640 名患者接受了经股颈动脉支架置入术。 匹配后,确定了 3286 对接受经颈动脉血运重建或经股动脉颈动脉支架置入术的患者(经颈动脉入路:平均 [SD] 年龄,71.7 [9.8] 岁;35.7% 为女性;经股动脉入路:平均 [SD] 年龄,71.6 [SD] 岁。 9.3] 年;35.1% 女性)。经颈动脉血运重建与较低的院内卒中或死亡风险相关(1.6% vs 3.1%;绝对差异,-1.52% [95% CI,-2.29% 至 -0.75%];相对风险 [RR],0.51 [95% CI,0.37 至 0.72];P < .001),卒中(1.3% 与 2.4%;绝对差异,-1.10% [95% CI,-1.79% 至 -0.41%];RR,0.54 [95% CI,0.38 至 0.79];P = 0.001)和死亡(0.4% 与 1.0%;绝对差异,-0.55% [95% CI,-0.98% 至 -0.11%];RR,0.44 [95% CI, 0.23 至 0.82];P = .008)。两个队列之间围手术期心肌梗死的风险没有统计学上的显着差异(经颈动脉入路为 0.2%,经股动脉入路为 0.3%;绝对差异,-0.09% [95% CI,-0.37% 至 0.19%];RR ,0.70 [95% CI,0.27 至 1.84];P = .47)。在使用 Kaplan-Meier 生命表估计的 1 年时,经颈动脉入路与同侧卒中或死亡风险较低相关(5.1% vs 9.6%;风险比,0.52 [95% CI,0.41 至 0.66];P < . 001)。经颈动脉血运重建与介入治疗导致的入路部位并发症风险较高相关(1.3% vs 0.8%;绝对差异,0.52% [95% CI,-0.01% 至 1.04%];RR,1.63 [95% CI,1.02]至 2.61];P = .04),而经股颈动脉支架置入术与更多辐射相关(中位透视时间,5 分钟 [四分位距 {IQR},3 至 7] 与 16 分钟 [IQR,11 至 23];P < .001) 和更多对比度(使用中值对比度,30 mL [IQR,20 至 45] 与 80 mL [IQR,55 至 122];P < .001)。结论和相关性 在接受颈动脉狭窄治疗的患者中,与经股颈动脉支架置入术相比,经颈动脉血运重建与较低的中风或死亡风险显着相关。
更新日期:2019-12-17
中文翻译:

经颈动脉血运重建与经股颈动脉支架置入术与颈动脉狭窄患者中风或死亡的关系
重要性 多项试验观察到,与颈动脉内膜切除术相比,经股颈动脉支架置入术围手术期卒中的发生率更高。最近引入了具有血流逆转的经颈动脉血运重建术用于颈动脉支架置入术。这项技术的开发是为了降低经股动脉入路的中风风险;然而,与经股颈动脉支架置入术相比,其结果尚不明确。目的 比较经颈动脉血运重建术和经股颈动脉支架置入术的相关结果。设计、设置和参与者 对美国和加拿大接受经颈动脉血运重建和经股颈动脉支架植入术的血管质量倡议经颈动脉监测项目和颈动脉支架登记处前瞻性收集的数据进行探索性倾向评分匹配分析。颈动脉狭窄,从2016年9月到2019年4月。最终随访日期是2019年5月29日。暴露经颈动脉血运重建与经股颈动脉支架置入术。主要结局和措施 结局包括院内卒中或死亡、卒中、死亡、心肌梗塞以及一年内同侧卒中或死亡的复合终点。院内卒中被定义为同侧或对侧、皮质或椎基底动脉、缺血性或出血性卒中。死亡是全因死亡率。结果 研究期间,5251 名患者接受了经颈动脉血运重建术,6640 名患者接受了经股颈动脉支架置入术。 匹配后,确定了 3286 对接受经颈动脉血运重建或经股动脉颈动脉支架置入术的患者(经颈动脉入路:平均 [SD] 年龄,71.7 [9.8] 岁;35.7% 为女性;经股动脉入路:平均 [SD] 年龄,71.6 [SD] 岁。 9.3] 年;35.1% 女性)。经颈动脉血运重建与较低的院内卒中或死亡风险相关(1.6% vs 3.1%;绝对差异,-1.52% [95% CI,-2.29% 至 -0.75%];相对风险 [RR],0.51 [95% CI,0.37 至 0.72];P < .001),卒中(1.3% 与 2.4%;绝对差异,-1.10% [95% CI,-1.79% 至 -0.41%];RR,0.54 [95% CI,0.38 至 0.79];P = 0.001)和死亡(0.4% 与 1.0%;绝对差异,-0.55% [95% CI,-0.98% 至 -0.11%];RR,0.44 [95% CI, 0.23 至 0.82];P = .008)。两个队列之间围手术期心肌梗死的风险没有统计学上的显着差异(经颈动脉入路为 0.2%,经股动脉入路为 0.3%;绝对差异,-0.09% [95% CI,-0.37% 至 0.19%];RR ,0.70 [95% CI,0.27 至 1.84];P = .47)。在使用 Kaplan-Meier 生命表估计的 1 年时,经颈动脉入路与同侧卒中或死亡风险较低相关(5.1% vs 9.6%;风险比,0.52 [95% CI,0.41 至 0.66];P < . 001)。经颈动脉血运重建与介入治疗导致的入路部位并发症风险较高相关(1.3% vs 0.8%;绝对差异,0.52% [95% CI,-0.01% 至 1.04%];RR,1.63 [95% CI,1.02]至 2.61];P = .04),而经股颈动脉支架置入术与更多辐射相关(中位透视时间,5 分钟 [四分位距 {IQR},3 至 7] 与 16 分钟 [IQR,11 至 23];P < .001) 和更多对比度(使用中值对比度,30 mL [IQR,20 至 45] 与 80 mL [IQR,55 至 122];P < .001)。结论和相关性 在接受颈动脉狭窄治疗的患者中,与经股颈动脉支架置入术相比,经颈动脉血运重建与较低的中风或死亡风险显着相关。











































 京公网安备 11010802027423号
京公网安备 11010802027423号