当前位置:
X-MOL 学术
›
Gastroenterology
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Incidence of Venous Thromboembolism in Patients With Newly Diagnosed Pancreatic Cancer and Factors Associated With Outcomes.
Gastroenterology ( IF 25.7 ) Pub Date : 2019-12-14 , DOI: 10.1053/j.gastro.2019.12.009 Corinne Frere 1 , Barbara Bournet 2 , Sophie Gourgou 3 , Julien Fraisse 3 , Cindy Canivet 2 , Jean M Connors 4 , Louis Buscail 2 , Dominique Farge 5 ,
Gastroenterology ( IF 25.7 ) Pub Date : 2019-12-14 , DOI: 10.1053/j.gastro.2019.12.009 Corinne Frere 1 , Barbara Bournet 2 , Sophie Gourgou 3 , Julien Fraisse 3 , Cindy Canivet 2 , Jean M Connors 4 , Louis Buscail 2 , Dominique Farge 5 ,
Affiliation
|
BACKGROUND & AIMS
Pancreatic ductal adenocarcinoma (PDAC) is associated with the highest incidence of venous thromboembolism (VTE) of any cancer type. However, little is known about risk factors for VTE or its outcomes in patients with PDAC.
METHODS
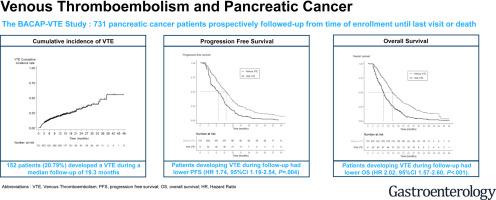
We collected data from a prospective, observational study performed at multiple centers in France from May 2014 through November 2018 (the Base Clinico-Biologique de l'Adénocarcinome Pancréatique [BACAP] study) linked to a database of patients with a new diagnosis of PDAC of any stage. Data were collected from 731 patients at baseline and during clinical follow-up or in the event of symptoms. The primary endpoint was the onset of VTE during follow-up. The secondary endpoints were progression-free survival (PFS) and overall survival (OS) times.
RESULTS
During a median follow-up of 19.3 months, 152 patients (20.79%) developed a VTE. The median time from PDAC diagnosis to the onset of VTE was 4.49 months. Cumulative incidence values of VTE were 8.07% (95% confidence interval [CI], 6.31-10.29) at 3 months and 19.21% (95% CI, 16.27-22.62) at 12 months. In multivariate analysis, PDAC primary tumor location (isthmus vs head: hazard ratio [HR], 2.06; 95% CI, 1.09-3.91; P = .027) and stage (locally advanced vs resectable or borderline: HR, 1.66; 95% CI, 1.10-2.51, P = .016; metastatic vs resectable or borderline: HR, 2.50; 95% CI, 1.64-3.79; P < .001) were independent risk factors for the onset of VTE. Patients who developed VTE during follow-up had shorter times of PFS (HR, 1.74; 95% CI, 1.19-2.54; P = .004) and OS (HR, 2.02; 95% CI, 1.57-2.60; P < .001).
CONCLUSION
In an analysis of data from the BACAP study, we found that frequent and early onsets of VTE after diagnoses of PDAC are associated with significant decreases in times of PFS and OS. Studies are needed to determine whether primary prophylaxis of VTE in patients with PDAC will improve morbidity and mortality related to VTE. (ClinicalTrials.gov, Number: clinicaltrials.gov as number NCT02818829).
中文翻译:

新诊断的胰腺癌和结果相关因素患者的静脉血栓栓塞发生率。
背景与目的胰腺导管腺癌(PDAC)与任何类型的癌症中静脉血栓栓塞(VTE)的发生率最高相关。但是,对于PDAC患者的VTE危险因素或其结果知之甚少。方法我们收集了2014年5月至2018年11月在法国多个中心进行的前瞻性观察性研究数据(基础临床胰腺癌生物学基础研究[BACAP]研究),该研究与具有PDAC新诊断的患者数据库相关联任何阶段。在基线,临床随访期间或出现症状时从731例患者中收集数据。主要终点是随访期间VTE的发作。次要终点是无进展生存期(PFS)和总生存期(OS)。结果在平均19.3个月的随访中,152例患者(20.79%)发生了VTE。从PDAC诊断到开始VTE的中位时间为4.49个月。3个月时VTE的累积发生值为8.07%(95%置信区间[CI],6.31-10.29),而12个月时VTE的累积发生值为19.21%(95%CI,16.27-22.62)。在多变量分析中,PDAC原发肿瘤的位置(峡部与头部:危险比[HR],2.06; 95%CI,1.09-3.91; P = .027)和分期(局部晚期与可切除或临界值:HR,1.66; 95% CI,1.10-2.51,P = .016;转移性与可切除性或临界值:HR,2.50; 95%CI,1.64-3.79; P <.001)是发生VTE的独立危险因素。随访期间发生VTE的患者的PFS(HR,1.74; 95%CI,1.19-2.54; P = .004)和OS(HR,2.02; 95%CI,1.57-2.60; P <.001)的时间较短。 )。结论在对BACAP研究数据的分析中,我们发现,在诊断出PDAC之后,VTE的频繁发作和早期发作与PFS和OS时间的显着减少有关。需要进行研究以确定对PDAC患者进行VTE的一级预防是否会改善与VTE相关的发病率和死亡率。(ClinicalTrials.gov,编号:clinicaltrials.gov,编号为NCT02818829)。
更新日期:2020-04-21
中文翻译:

新诊断的胰腺癌和结果相关因素患者的静脉血栓栓塞发生率。
背景与目的胰腺导管腺癌(PDAC)与任何类型的癌症中静脉血栓栓塞(VTE)的发生率最高相关。但是,对于PDAC患者的VTE危险因素或其结果知之甚少。方法我们收集了2014年5月至2018年11月在法国多个中心进行的前瞻性观察性研究数据(基础临床胰腺癌生物学基础研究[BACAP]研究),该研究与具有PDAC新诊断的患者数据库相关联任何阶段。在基线,临床随访期间或出现症状时从731例患者中收集数据。主要终点是随访期间VTE的发作。次要终点是无进展生存期(PFS)和总生存期(OS)。结果在平均19.3个月的随访中,152例患者(20.79%)发生了VTE。从PDAC诊断到开始VTE的中位时间为4.49个月。3个月时VTE的累积发生值为8.07%(95%置信区间[CI],6.31-10.29),而12个月时VTE的累积发生值为19.21%(95%CI,16.27-22.62)。在多变量分析中,PDAC原发肿瘤的位置(峡部与头部:危险比[HR],2.06; 95%CI,1.09-3.91; P = .027)和分期(局部晚期与可切除或临界值:HR,1.66; 95% CI,1.10-2.51,P = .016;转移性与可切除性或临界值:HR,2.50; 95%CI,1.64-3.79; P <.001)是发生VTE的独立危险因素。随访期间发生VTE的患者的PFS(HR,1.74; 95%CI,1.19-2.54; P = .004)和OS(HR,2.02; 95%CI,1.57-2.60; P <.001)的时间较短。 )。结论在对BACAP研究数据的分析中,我们发现,在诊断出PDAC之后,VTE的频繁发作和早期发作与PFS和OS时间的显着减少有关。需要进行研究以确定对PDAC患者进行VTE的一级预防是否会改善与VTE相关的发病率和死亡率。(ClinicalTrials.gov,编号:clinicaltrials.gov,编号为NCT02818829)。











































 京公网安备 11010802027423号
京公网安备 11010802027423号