当前位置:
X-MOL 学术
›
Kidney Int.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
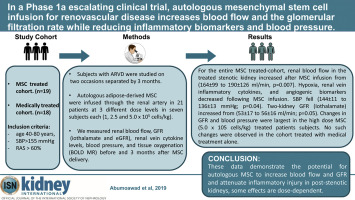
In a Phase 1a escalating clinical trial, autologous mesenchymal stem cell infusion for renovascular disease increases blood flow and the glomerular filtration rate while reducing inflammatory biomarkers and blood pressure.
Kidney International ( IF 14.8 ) Pub Date : 2019-12-13 , DOI: 10.1016/j.kint.2019.11.022 Abdelrhman Abumoawad 1 , Ahmed Saad 2 , Christopher M Ferguson 1 , Alfonso Eirin 1 , Sandra M Herrmann 1 , LaTonya J Hickson 1 , Busra B Goksu 1 , Emily Bendel 3 , Sanjay Misra 3 , James Glockner 3 , Allan B Dietz 4 , Lilach O Lerman 1 , Stephen C Textor 1
Kidney International ( IF 14.8 ) Pub Date : 2019-12-13 , DOI: 10.1016/j.kint.2019.11.022 Abdelrhman Abumoawad 1 , Ahmed Saad 2 , Christopher M Ferguson 1 , Alfonso Eirin 1 , Sandra M Herrmann 1 , LaTonya J Hickson 1 , Busra B Goksu 1 , Emily Bendel 3 , Sanjay Misra 3 , James Glockner 3 , Allan B Dietz 4 , Lilach O Lerman 1 , Stephen C Textor 1
Affiliation
|
Atherosclerotic renovascular disease (ARVD) reduces tissue perfusion and eventually leads to loss of kidney function with limited therapeutic options. Here we describe results of Phase 1a escalating dose clinical trial of autologous mesenchymal stem cell infusion for ARVD. Thirty-nine patients with ARVD were studied on two occasions separated by three months. Autologous adipose-derived mesenchymal stem cells were infused through the renal artery in 21 patients at three different dose levels (1, 2.5 and 5.0 × 105 cells/kg) in seven patients each. We measured renal blood flow, glomerular filtration rate (GFR) (iothalamate and estimated GFR), renal vein cytokine levels, blood pressure, and tissue oxygenation before and three months after stem cell delivery. These indices were compared to those of 18 patients with ARVD matched for age, kidney function and blood pressure receiving medical therapy alone that underwent an identical study protocol. Cultured mesenchymal stem cells were also studied in vitro. For the entire stem cell treated-cohort, mean renal blood flow in the treated stenotic kidney significantly increased after stem cell infusion from (164 to 190 ml/min). Hypoxia, renal vein inflammatory cytokines, and angiogenic biomarkers significantly decreased following stem cell infusion. Mean systolic blood pressure significantly fell (144 to 136 mmHg) and the mean two-kidney GFR (Iothalamate) modestly but significantly increased from (53 to 56 ml/min). Changes in GFR and blood pressure were largest in the high dose stem cell treated individuals. No such changes were observed in the cohort receiving medical treatment alone. Thus, our data demonstrate the potential for autologous mesenchymal stem cell to increase blood flow, GFR and attenuate inflammatory injury in post-stenotic kidneys. The observation that some effects are dose-dependent and related to in-vitro properties of mesenchymal stem cell may direct efforts to maximize potential therapeutic efficacy.
中文翻译:

在一项 1a 期逐步升级的临床试验中,自体间充质干细胞输注治疗肾血管疾病可增加血流量和肾小球滤过率,同时降低炎症生物标志物和血压。
动脉粥样硬化性肾血管疾病(ARVD)会减少组织灌注,最终导致肾功能丧失,而治疗选择有限。在这里,我们描述了自体间充质干细胞输注治疗 ARVD 的 1a 期剂量递增临床试验的结果。对 39 名 ARVD 患者进行了两次研究,间隔三个月。通过肾动脉将自体脂肪间充质干细胞以三种不同剂量水平(1、2.5 和 5.0 × 105 个细胞/kg)输注到 21 名患者中,每组 7 名患者。我们在干细胞移植前和移植后三个月测量了肾血流量、肾小球滤过率 (GFR)(碘酞酸盐和估计 GFR)、肾静脉细胞因子水平、血压和组织氧合。这些指数与 18 名年龄、肾功能和血压相匹配的 ARVD 患者进行了比较,这些患者接受了相同的研究方案,仅接受药物治疗。还对培养的间充质干细胞进行了体外研究。对于整个干细胞治疗组,干细胞输注后,治疗后狭窄肾脏的平均肾血流量显着增加(从 164 毫升/分钟增加到 190 毫升/分钟)。干细胞输注后,缺氧、肾静脉炎症细胞因子和血管生成生物标志物显着减少。平均收缩压显着下降(从 144 毫米汞柱降至 136 毫米汞柱),平均两肾肾小球滤过率(碘沙拉酯)略有增加,但显着增加(从 53 毫升/分钟升至 56 毫升/分钟)。高剂量干细胞治疗个体的 GFR 和血压变化最大。在仅接受药物治疗的队列中没有观察到此类变化。因此,我们的数据证明自体间充质干细胞具有增加血流量、GFR 和减轻狭窄后肾脏炎症损伤的潜力。一些效应是剂量依赖性的并且与间充质干细胞的体外特性相关的观察结果可能会指导努力最大化潜在的治疗功效。
更新日期:2019-12-13
中文翻译:

在一项 1a 期逐步升级的临床试验中,自体间充质干细胞输注治疗肾血管疾病可增加血流量和肾小球滤过率,同时降低炎症生物标志物和血压。
动脉粥样硬化性肾血管疾病(ARVD)会减少组织灌注,最终导致肾功能丧失,而治疗选择有限。在这里,我们描述了自体间充质干细胞输注治疗 ARVD 的 1a 期剂量递增临床试验的结果。对 39 名 ARVD 患者进行了两次研究,间隔三个月。通过肾动脉将自体脂肪间充质干细胞以三种不同剂量水平(1、2.5 和 5.0 × 105 个细胞/kg)输注到 21 名患者中,每组 7 名患者。我们在干细胞移植前和移植后三个月测量了肾血流量、肾小球滤过率 (GFR)(碘酞酸盐和估计 GFR)、肾静脉细胞因子水平、血压和组织氧合。这些指数与 18 名年龄、肾功能和血压相匹配的 ARVD 患者进行了比较,这些患者接受了相同的研究方案,仅接受药物治疗。还对培养的间充质干细胞进行了体外研究。对于整个干细胞治疗组,干细胞输注后,治疗后狭窄肾脏的平均肾血流量显着增加(从 164 毫升/分钟增加到 190 毫升/分钟)。干细胞输注后,缺氧、肾静脉炎症细胞因子和血管生成生物标志物显着减少。平均收缩压显着下降(从 144 毫米汞柱降至 136 毫米汞柱),平均两肾肾小球滤过率(碘沙拉酯)略有增加,但显着增加(从 53 毫升/分钟升至 56 毫升/分钟)。高剂量干细胞治疗个体的 GFR 和血压变化最大。在仅接受药物治疗的队列中没有观察到此类变化。因此,我们的数据证明自体间充质干细胞具有增加血流量、GFR 和减轻狭窄后肾脏炎症损伤的潜力。一些效应是剂量依赖性的并且与间充质干细胞的体外特性相关的观察结果可能会指导努力最大化潜在的治疗功效。









































 京公网安备 11010802027423号
京公网安备 11010802027423号