当前位置:
X-MOL 学术
›
Hypertens. Res.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Nocturnal blood pressure patterns and cardiac damage: there is still much to learn
Hypertension Research ( IF 4.3 ) Pub Date : 2019-12-12 , DOI: 10.1038/s41440-019-0372-x Domenico Di Raimondo 1 , Gaia Musiari 1 , Antonio Pinto 1
Hypertension Research ( IF 4.3 ) Pub Date : 2019-12-12 , DOI: 10.1038/s41440-019-0372-x Domenico Di Raimondo 1 , Gaia Musiari 1 , Antonio Pinto 1
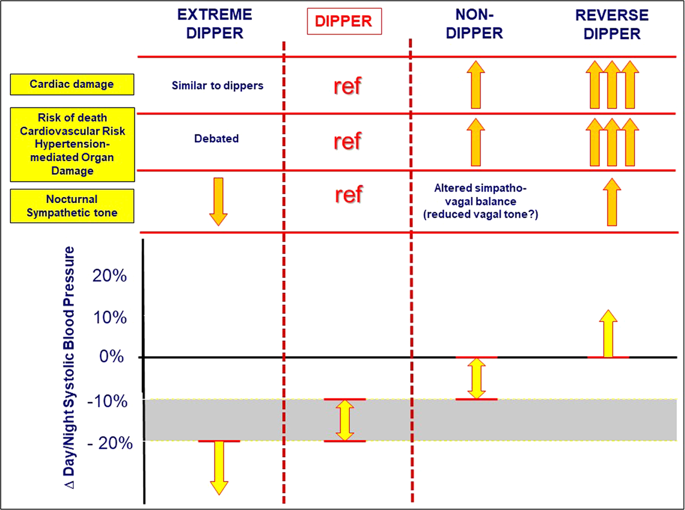
Affiliation
|
Most normotensive and hypertensive subjects show a physiologic reduction in blood pressure (BP) during sleep. However, a minority of subjects show a blunted or exaggerated nocturnal BP reduction or even a paradoxical increase in BP. Over the past 30 years, 24-h ambulatory blood pressure monitoring (ABPM) has been suggested to be the recommended technique for out-of-office BP measurements, helping to significantly improve the clinical management of hypertension, precisely because it may provide several pieces of information regarding nocturnal BP levels otherwise not available [1]. Ascertaining whether the “dipping” status (i.e., the nocturnal decline in BP) is maintained or the circadian rhythm of BP is altered (falling into one of the three alternative nocturnal BP patterns described as nondipping, extreme dipping and reverse dipping) (see Fig. 1) is highly relevant since both the dipping status and the related night/day BP ratio are recognized as better predictors of all-cause mortality and adverse cardiovascular (CV) outcomes than inoffice BP or daytime ambulatory BP [1]. An impressive amount of evidence based on several well-designed prospective studies has confirm that a reduced nocturnal BP decline has been associated with a high risk of death, with a poor CV outcome and highly advanced target organ damage [2]. Trying to classify hypertensive individuals into subgroups based on their nocturnal BP patterns is not free of criticism, the most relevant of which is the poor reproducibility of the dipping status [2]. Furthermore, there are substantial methodological issues due to the dichotomic classification of dipping/nondipping often used in papers, which appears to be much less specific in predicting CV outcomes than the classification with four patterns [3]. When considering four dipping subgroups, the responsibility for a very substantial percentage of those with the nondipping pattern who have the worst prognoses (for all outcomes) is attributable to reverse dippers [2]. On the other hand, extreme dippers seem to have little or no risk, showing a good prognostic value that is as good as those with a dipping pattern, if not better, [3–5] making the actual prognostic value of extreme dipping worthy of targeted analyses. Note that a consistent part of the cardio and cerebrovascular risk ascribed to the extreme dipping pattern may be related to nocturnal recurrent episodes of low BP exacerbated by an inappropriate dose of antihypertensive therapy at bedtime. This risk further underlines the importance of establishing the nocturnal BP pattern before setting a drug therapy regimen, especially in the highly fragile categories of patients (those with elderly, secondary prevention of chronic coronary syndromes, acute and chronic cerebrovascular diseases) [3, 5]. The assessment of hypertensive heart disease was often limited to an analysis of the direct consequences of the chronically increased afterload on left ventricular (LV) chambers, leading to LV hypertrophy, left atrial enlargement, and LV systolic and diastolic dysfunction, all of which are risk factors for the development of heart failure and atrial arrhythmias. Recently, a study of the complex and various influences on cardiac structure and function that occur secondary to prolonged untreated systemic hypertension has led to the observation that the right heart is often affected, although the right chambers are not directly exposed to the chronic increase in the systemic afterload, and the architecture and the pattern of contractions is intrinsically different between the right and left ventricles. The involvement of the right ventricle (RV) and then atrium is pathophysiologically justified by mechanic causes (mainly through the interventricular septum remodeling that leads to a direct left-to-right transmission of the systemic afterload) and by the neurohumoral activation induced by * Domenico Di Raimondo domenico.diraimondo@unipa.it
中文翻译:

夜间血压模式和心脏损伤:还有很多东西需要学习
大多数血压正常和高血压的受试者在睡眠期间表现出生理性血压 (BP) 降低。然而,少数受试者表现出夜间血压降低或什至自相矛盾的升高。在过去的 30 年中,24 小时动态血压监测 (ABPM) 被建议作为诊室外血压测量的推荐技术,有助于显着改善高血压的临床管理,正是因为它可以提供几个部分有关夜间血压水平的信息,否则无法获得 [1]。确定是否维持“浸渍”状态(即夜间血压下降)或改变血压的昼夜节律(落入被描述为非浸渍、极度浸渍和反向浸渍的三种替代的夜间血压模式之一)(见图) . 1) 高度相关,因为与办公室血压或白天动态血压相比,浸渍状态和相关的夜间/白天血压比被认为是全因死亡率和不良心血管 (CV) 结果的更好预测因子 [1]。基于几项精心设计的前瞻性研究的大量证据证实,夜间血压下降减少与死亡风险高、心血管结局差和靶器官损伤高度严重相关 [2]。试图根据他们的夜间血压模式将高血压个体分为亚组并非没有批评,其中最相关的是浸渍状态的可重复性较差 [2]。此外,由于论文中经常使用浸渍/非浸渍的二分法,存在大量的方法学问题,与四种模式的分类相比,这似乎在预测 CV 结果方面的特异性要低得多 [3]。在考虑四个浸渍亚组时,有很大比例的非浸渍型患者预后最差(对于所有结果)可归因于反向浸渍型 [2]。另一方面,极端倾角似乎风险很小或没有风险,显示出与具有倾角模式的那些一样好,甚至更好的良好预后值,[3-5] 使得极端倾角的实际预测值值得针对性分析。请注意,归因于极端浸渍模式的心血管和脑血管风险的一致部分可能与夜间反复发作的低血压有关,而在睡前不适当剂量的抗高血压治疗会加剧这种情况。这种风险进一步强调了在制定药物治疗方案之前确定夜间血压模式的重要性,尤其是在高度脆弱的患者中(老年人、慢性冠状动脉综合征的二级预防、急性和慢性脑血管疾病)[3, 5] . 高血压心脏病的评估通常仅限于分析左心室 (LV) 腔室长期后负荷增加的直接后果,导致 LV 肥厚、左心房扩大以及 LV 收缩和舒张功能障碍,所有这些都是风险心力衰竭和房性心律失常发生的因素。最近,对长期未经治疗的全身性高血压继发于心脏结构和功能的复杂和各种影响的研究导致观察到右心经常受到影响,尽管右心室没有直接暴露于全身后负荷的慢性增加,并且右心室和左心室之间的结构和收缩模式本质上是不同的。右心室 (RV) 和心房受累在病理生理学上是由机械原因(主要通过导致全身后负荷从左向右直接传递的室间隔重塑)和由 * Domenico 诱导的神经体液激活所证明的Di Raimondo domenico.diraimondo@unipa.it 尽管右心室不会直接暴露于全身后负荷的慢性增加,而且右心室和左心室的结构和收缩模式本质上是不同的。右心室 (RV) 和心房受累在病理生理学上是由机械原因(主要通过室间隔重塑导致全身后负荷从左向右直接传递)和由 * Domenico 诱导的神经体液激活所证明的Di Raimondo domenico.diraimondo@unipa.it 尽管右心室不会直接暴露于全身后负荷的慢性增加,而且右心室和左心室的结构和收缩模式本质上是不同的。右心室 (RV) 和心房受累在病理生理学上是由机械原因(主要通过室间隔重塑导致全身后负荷从左向右直接传递)和由 * Domenico 诱导的神经体液激活所证明的Di Raimondo domenico.diraimondo@unipa.it
更新日期:2019-12-12
中文翻译:

夜间血压模式和心脏损伤:还有很多东西需要学习
大多数血压正常和高血压的受试者在睡眠期间表现出生理性血压 (BP) 降低。然而,少数受试者表现出夜间血压降低或什至自相矛盾的升高。在过去的 30 年中,24 小时动态血压监测 (ABPM) 被建议作为诊室外血压测量的推荐技术,有助于显着改善高血压的临床管理,正是因为它可以提供几个部分有关夜间血压水平的信息,否则无法获得 [1]。确定是否维持“浸渍”状态(即夜间血压下降)或改变血压的昼夜节律(落入被描述为非浸渍、极度浸渍和反向浸渍的三种替代的夜间血压模式之一)(见图) . 1) 高度相关,因为与办公室血压或白天动态血压相比,浸渍状态和相关的夜间/白天血压比被认为是全因死亡率和不良心血管 (CV) 结果的更好预测因子 [1]。基于几项精心设计的前瞻性研究的大量证据证实,夜间血压下降减少与死亡风险高、心血管结局差和靶器官损伤高度严重相关 [2]。试图根据他们的夜间血压模式将高血压个体分为亚组并非没有批评,其中最相关的是浸渍状态的可重复性较差 [2]。此外,由于论文中经常使用浸渍/非浸渍的二分法,存在大量的方法学问题,与四种模式的分类相比,这似乎在预测 CV 结果方面的特异性要低得多 [3]。在考虑四个浸渍亚组时,有很大比例的非浸渍型患者预后最差(对于所有结果)可归因于反向浸渍型 [2]。另一方面,极端倾角似乎风险很小或没有风险,显示出与具有倾角模式的那些一样好,甚至更好的良好预后值,[3-5] 使得极端倾角的实际预测值值得针对性分析。请注意,归因于极端浸渍模式的心血管和脑血管风险的一致部分可能与夜间反复发作的低血压有关,而在睡前不适当剂量的抗高血压治疗会加剧这种情况。这种风险进一步强调了在制定药物治疗方案之前确定夜间血压模式的重要性,尤其是在高度脆弱的患者中(老年人、慢性冠状动脉综合征的二级预防、急性和慢性脑血管疾病)[3, 5] . 高血压心脏病的评估通常仅限于分析左心室 (LV) 腔室长期后负荷增加的直接后果,导致 LV 肥厚、左心房扩大以及 LV 收缩和舒张功能障碍,所有这些都是风险心力衰竭和房性心律失常发生的因素。最近,对长期未经治疗的全身性高血压继发于心脏结构和功能的复杂和各种影响的研究导致观察到右心经常受到影响,尽管右心室没有直接暴露于全身后负荷的慢性增加,并且右心室和左心室之间的结构和收缩模式本质上是不同的。右心室 (RV) 和心房受累在病理生理学上是由机械原因(主要通过导致全身后负荷从左向右直接传递的室间隔重塑)和由 * Domenico 诱导的神经体液激活所证明的Di Raimondo domenico.diraimondo@unipa.it 尽管右心室不会直接暴露于全身后负荷的慢性增加,而且右心室和左心室的结构和收缩模式本质上是不同的。右心室 (RV) 和心房受累在病理生理学上是由机械原因(主要通过室间隔重塑导致全身后负荷从左向右直接传递)和由 * Domenico 诱导的神经体液激活所证明的Di Raimondo domenico.diraimondo@unipa.it 尽管右心室不会直接暴露于全身后负荷的慢性增加,而且右心室和左心室的结构和收缩模式本质上是不同的。右心室 (RV) 和心房受累在病理生理学上是由机械原因(主要通过室间隔重塑导致全身后负荷从左向右直接传递)和由 * Domenico 诱导的神经体液激活所证明的Di Raimondo domenico.diraimondo@unipa.it











































 京公网安备 11010802027423号
京公网安备 11010802027423号