The Lancet Global Health ( IF 19.9 ) Pub Date : 2019-12-11 , DOI: 10.1016/s2214-109x(19)30463-2 Adam Wagstaff 1 , Sven Neelsen 2
|
Background
The goal of universal health coverage (UHC) requires that everyone receive needed health services, and that families who get needed services do not suffer undue financial hardship. Tracking progress towards UHC requires measurement of both these dimensions, and a way of trading them off against one another.
Methods
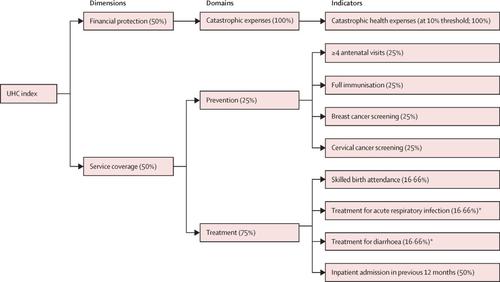
We measured service coverage by a weighted geometric average of four prevention indicators (antenatal care, full immunisation, and screening for breast and cervical cancers) and four treatment indicators (skilled birth attendance, inpatient admission, and treatment for acute respiratory infection and diarrhoea), financial protection by the incidence of catastrophic health expenditures (those exceeding 10% of household consumption or income), and a country's UHC performance as a geometric average of the service coverage index and the complement of the incidence of catastrophic expenditures. Where possible, we adjusted service coverage for inequality, penalising countries with a high level of inequality. The bulk of data used in this study were from the World Bank's Health Equity and Financial Protection Indicators database (2019 version), comprising data from household surveys. Gaps in the data were supplemented with other survey data and (where necessary) non-survey data from other sources (administrative, modelled, and imputed data).
Findings
A low incidence of catastrophic expenses sometimes reflects low service coverage (often in low-income countries) but sometimes occurs despite high service coverage (often in high-income countries). At a given level of service coverage, financial protection also varies. UHC index scores are generally higher in higher-income countries, but there are variations within income groups. Adjusting the UHC index for inequality in service coverage makes little difference in some countries, but reduces it by more than 10% in others. Seven of the 12 countries for which we were able to produce trend data have increased their UHC index over time (with the greatest average yearly increases seen in Ghana [1·43%], Indonesia [1·85%], and Vietnam [2·26%]), mostly by improving both financial protection and service coverage. Some increased their UHC index, despite reductions in financial protection, by substantially increasing their service coverage. The UHC index decreased in five of 12 countries with trend data, mostly because financial protection worsened with stagnant or declining service coverage. Our UHC indicators (except inpatient admissions) are significantly and positively associated with GDP per capita, and most are correlated with the share of health spending channelled through social health insurance and government schemes. However, associations of our UHC indicators with the share of GDP spent on health and the shares of health spending channelled through non-profit and private insurance are ambiguous.
Interpretation
Progress towards UHC can be tracked using an index that captures both service coverage and financial protection. Although per-capita income is a good predictor of a country's UHC index score, some countries perform better than others in the same income group or even in the income group above their own. Strong UHC performance is correlated with the share of a country's health budget that is channelled through government and social health insurance schemes.
Funding
None.
中文翻译:

对111个国家的全民健康覆盖范围的全面评估:一项回顾性观察研究。
背景
全民健康覆盖(UHC)的目标要求每个人都获得所需的卫生服务,并且获得所需服务的家庭不会遭受不必要的经济困难。追踪实现UHC的进度需要同时衡量这两个方面,并需要权衡取舍。
方法
我们用四个预防指标(产前保健,全面免疫和筛查乳腺癌和宫颈癌)和四个治疗指标(熟练接生,住院率以及急性呼吸道感染和腹泻的治疗)的加权几何平均值来衡量服务覆盖率,灾难性医疗支出(超过家庭消费或收入的10%)的发生率,以及一国的UHC绩效(服务覆盖率指数的几何平均值)和灾难性支出发生率的补充,从而提供财务保护。在可能的情况下,我们针对不平等情况调整了服务范围,对不平等程度较高的国家进行了惩罚。本研究中使用的大量数据来自世界银行的健康公平与金融保护指标数据库(2019年版),包括来自家庭调查的数据。数据中的空白被其他调查数据和(必要时)来自其他来源的非调查数据(行政数据,模型数据和估算数据)补充。
发现
灾难性支出的低发生率有时反映了服务覆盖率低(通常在低收入国家/地区),但有时却发生在服务覆盖率高的情况下(通常在高收入国家/地区)。在给定的服务范围内,财务保护也会有所不同。在收入较高的国家,UHC指数得分通常较高,但是收入组之间存在差异。调整UHC指数以实现服务覆盖率不平等在某些国家几乎没有影响,但在其他国家则减少了10%以上。我们能够提供趋势数据的12个国家中,有7个国家的UHC指数随着时间的推移而增加(加纳[1·43%],印度尼西亚[1·85%]和越南[2]的年均增幅最大) ·[26%]),主要是通过同时改善财务保护和服务覆盖率。有些增加了他们的UHC指数,尽管减少了财务保护,但仍通过大幅增加其服务覆盖面来实现。在具有趋势数据的12个国家中,有5个国家的UHC指数有所下降,这主要是因为金融保护因服务覆盖率停滞或下降而恶化。我们的UHC指标(住院患者除外)与人均GDP呈显着正相关,并且大多数与通过社会医疗保险和政府计划提供的医疗支出份额相关。但是,我们的UHC指标与医疗保健支出占GDP的比例以及通过非营利和私人保险渠道转移的医疗保健支出的比例之间的关系不明确。主要是由于服务覆盖率停滞或下降而导致金融保护恶化。我们的UHC指标(住院患者除外)与人均GDP呈显着正相关,并且大多数与通过社会医疗保险和政府计划提供的医疗支出份额相关。但是,我们的UHC指标与医疗保健支出占GDP的比例以及通过非营利和私人保险渠道转移的医疗保健支出的比例之间的关系不明确。主要是由于服务覆盖率停滞或下降而导致金融保护恶化。我们的UHC指标(住院患者除外)与人均GDP呈显着正相关,并且大多数与通过社会医疗保险和政府计划提供的医疗支出份额相关。但是,我们的UHC指标与医疗保健支出占GDP的比例以及通过非营利和私人保险渠道转移的医疗保健支出的比例之间的关系不明确。
解释
可以使用同时涵盖服务范围和财务保护的索引来跟踪实现UHC的进度。尽管人均收入可以很好地预测一个国家的UHC指数得分,但在同一个收入组甚至高于其本国的收入组中,有些国家的表现要好于其他国家。UHC的强劲表现与通过政府和社会健康保险计划提供的国家健康预算的份额相关。
资金
没有。











































 京公网安备 11010802027423号
京公网安备 11010802027423号