当前位置:
X-MOL 学术
›
JACC Cardiovasc. Inte.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Effect of Oxygen Therapy on Cardiovascular Outcomes in Relation to Baseline Oxygen Saturation.
JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2019-12-11 , DOI: 10.1016/j.jcin.2019.09.016 Stefan K James 1 , David Erlinge 2 , Johan Herlitz 3 , Joakim Alfredsson 4 , Sasha Koul 2 , Ole Fröbert 5 , Thomas Kellerth 5 , Annica Ravn-Fischer 6 , Patrik Alström 7 , Ollie Östlund 8 , Tomas Jernberg 9 , Bertil Lindahl 1 , Robin Hofmann 7 ,
JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2019-12-11 , DOI: 10.1016/j.jcin.2019.09.016 Stefan K James 1 , David Erlinge 2 , Johan Herlitz 3 , Joakim Alfredsson 4 , Sasha Koul 2 , Ole Fröbert 5 , Thomas Kellerth 5 , Annica Ravn-Fischer 6 , Patrik Alström 7 , Ollie Östlund 8 , Tomas Jernberg 9 , Bertil Lindahl 1 , Robin Hofmann 7 ,
Affiliation
|
OBJECTIVES
The aim of this study was to determine the effect of supplemental oxygen in patients with myocardial infarction (MI) on the composite of all-cause death, rehospitalization with MI, or heart failure related to baseline oxygen saturation. A secondary objective was to investigate outcomes in patients developing hypoxemia.
BACKGROUND
In the DETO2X-AMI (Determination of the Role of Oxygen in Suspected Acute Myocardial Infarction) trial, 6,629 normoxemic patients with suspected MI were randomized to oxygen at 6 l/min for 6 to 12 h or ambient air.
METHODS
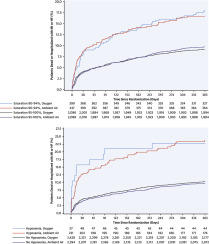
The study population of 5,010 patients with confirmed MI was divided by baseline oxygen saturation into a low-normal (90% to 94%) and a high-normal (95% to 100%) cohort. Outcomes are reported within 1 year. To increase power, all follow-up time (between 1 and 4 years) was included post hoc, and interaction analyses were performed with oxygen saturation as a continuous covariate.
RESULTS
The composite endpoint of all-cause death, rehospitalization with MI, or heart failure occurred significantly more often in patients in the low-normal cohort (17.3%) compared with those in the high-normal cohort (9.5%) (p < 0.001), and most often in patients developing hypoxemia (23.6%). Oxygen therapy compared with ambient air was not associated with improved outcomes regardless of baseline oxygen saturation (interaction p values: composite endpoint, p = 0.79; all-cause death, p = 0.33; rehospitalization with MI, p = 0.86; hospitalization for heart failure, p = 0.35).
CONCLUSIONS
Irrespective of oxygen saturation at baseline, we found no clinically relevant beneficial effect of routine oxygen therapy in normoxemic patients with MI regarding cardiovascular outcomes. Low-normal baseline oxygen saturation or development of hypoxemia was identified as an independent marker of poor prognosis. (An Efficacy and Outcome Study of Supplemental Oxygen Treatment in Patients With Suspected Myocardial Infarction; NCT01787110).
中文翻译:

氧疗法对与基线氧饱和度有关的心血管结果的影响。
目的本研究的目的是确定心肌梗死(MI)患者补充氧气对全因死亡,MI再次住院或与基线氧饱和度相关的心力衰竭的综合影响。次要目标是研究低氧血症患者的预后。背景技术在DETO2X-AMI(确定可疑急性心肌梗死中氧气的作用)试验中,将6629名可疑MI的高氧血症患者随机分配为6 l / min的氧气持续6至12 h或周围空气。方法研究人群中5,010例确诊为MI的患者按基线血氧饱和度分为低正常人群(90%至94%)和高正常人群(95%至100%)。结果在1年内报告。为了提高能力,事后包括了所有的随访时间(1至4年),并以氧饱和度作为连续协变量进行相互作用分析。结果低正常组(17.3%)患者的全因死亡,心梗再入院或心力衰竭的复合终点发生率显着高于高正常组(9.5%)(p <0.001) ),最常见于发生低氧血症的患者(23.6%)。不论基线氧饱和度如何,与周围空气相比,氧疗与改善结局均无相关性(相互作用p值:复合终点,p = 0.79;全因死亡,p = 0.33; MI入院,p = 0.86;心力衰竭住院,p = 0.35)。结论无论基线氧饱和度如何,我们发现常规血氧疗法对心律不齐的MI患者在心血管结局方面无临床意义的有益作用。低正常基线血氧饱和度或低氧血症的发展被认为是预后不良的独立标志。(疑似心肌梗死患者补充氧气治疗的疗效和结果研究; NCT01787110)。
更新日期:2019-12-11
中文翻译:

氧疗法对与基线氧饱和度有关的心血管结果的影响。
目的本研究的目的是确定心肌梗死(MI)患者补充氧气对全因死亡,MI再次住院或与基线氧饱和度相关的心力衰竭的综合影响。次要目标是研究低氧血症患者的预后。背景技术在DETO2X-AMI(确定可疑急性心肌梗死中氧气的作用)试验中,将6629名可疑MI的高氧血症患者随机分配为6 l / min的氧气持续6至12 h或周围空气。方法研究人群中5,010例确诊为MI的患者按基线血氧饱和度分为低正常人群(90%至94%)和高正常人群(95%至100%)。结果在1年内报告。为了提高能力,事后包括了所有的随访时间(1至4年),并以氧饱和度作为连续协变量进行相互作用分析。结果低正常组(17.3%)患者的全因死亡,心梗再入院或心力衰竭的复合终点发生率显着高于高正常组(9.5%)(p <0.001) ),最常见于发生低氧血症的患者(23.6%)。不论基线氧饱和度如何,与周围空气相比,氧疗与改善结局均无相关性(相互作用p值:复合终点,p = 0.79;全因死亡,p = 0.33; MI入院,p = 0.86;心力衰竭住院,p = 0.35)。结论无论基线氧饱和度如何,我们发现常规血氧疗法对心律不齐的MI患者在心血管结局方面无临床意义的有益作用。低正常基线血氧饱和度或低氧血症的发展被认为是预后不良的独立标志。(疑似心肌梗死患者补充氧气治疗的疗效和结果研究; NCT01787110)。











































 京公网安备 11010802027423号
京公网安备 11010802027423号