Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Homogeneity in the association of body mass index with type 2 diabetes across the UK Biobank: A Mendelian randomization study.
PLOS Medicine ( IF 10.5 ) Pub Date : 2019-12-10 , DOI: 10.1371/journal.pmed.1002982 Michael Wainberg 1 , Anubha Mahajan 2, 3 , Anshul Kundaje 1, 4 , Mark I McCarthy 2, 3, 5 , Erik Ingelsson 6, 7, 8, 9 , Nasa Sinnott-Armstrong 4 , Manuel A Rivas 10
PLOS Medicine ( IF 10.5 ) Pub Date : 2019-12-10 , DOI: 10.1371/journal.pmed.1002982 Michael Wainberg 1 , Anubha Mahajan 2, 3 , Anshul Kundaje 1, 4 , Mark I McCarthy 2, 3, 5 , Erik Ingelsson 6, 7, 8, 9 , Nasa Sinnott-Armstrong 4 , Manuel A Rivas 10
Affiliation
|
BACKGROUND
Lifestyle interventions to reduce body mass index (BMI) are critical public health strategies for type 2 diabetes prevention. While weight loss interventions have shown demonstrable benefit for high-risk and prediabetic individuals, we aimed to determine whether the same benefits apply to those at lower risk.
METHODS AND FINDINGS
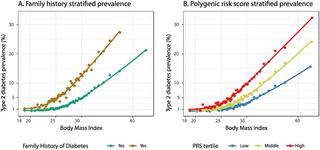
We performed a multi-stratum Mendelian randomization study of the effect size of BMI on diabetes odds in 287,394 unrelated individuals of self-reported white British ancestry in the UK Biobank, who were recruited from across the United Kingdom from 2006 to 2010 when they were between the ages of 40 and 69 years. Individuals were stratified on the following diabetes risk factors: BMI, diabetes family history, and genome-wide diabetes polygenic risk score. The main outcome measure was the odds ratio of diabetes per 1-kg/m2 BMI reduction, in the full cohort and in each stratum. Diabetes prevalence increased sharply with BMI, family history of diabetes, and genetic risk. Conversely, predicted risk reduction from weight loss was strikingly similar across BMI and genetic risk categories. Weight loss was predicted to substantially reduce diabetes odds even among lower-risk individuals: for instance, a 1-kg/m2 BMI reduction was associated with a 1.37-fold reduction (95% CI 1.12-1.68) in diabetes odds among non-overweight individuals (BMI < 25 kg/m2) without a family history of diabetes, similar to that in obese individuals (BMI ≥ 30 kg/m2) with a family history (1.21-fold reduction, 95% CI 1.13-1.29). A key limitation of this analysis is that the BMI-altering DNA sequence polymorphisms it studies represent cumulative predisposition over an individual's entire lifetime, and may consequently incorrectly estimate the risk modification potential of weight loss interventions later in life.
CONCLUSIONS
In a population-scale cohort, lower BMI was consistently associated with reduced diabetes risk across BMI, family history, and genetic risk categories, suggesting all individuals can substantially reduce their diabetes risk through weight loss. Our results support the broad deployment of weight loss interventions to individuals at all levels of diabetes risk.
中文翻译:

英国生物银行体重指数与 2 型糖尿病关联的同质性:孟德尔随机研究。
背景技术降低体重指数(BMI)的生活方式干预是预防2型糖尿病的关键公共卫生策略。虽然减肥干预措施对高风险和糖尿病前期个体显示出明显的益处,但我们的目的是确定同样的益处是否适用于低风险人群。方法和结果 我们对英国生物库中 287,394 名自报的英国白人血统的无关个体进行了一项多层次孟德尔随机化研究,研究 BMI 对糖尿病几率的影响大小,这些个体于 2006 年至 2010 年期间从英国各地招募,当时他们的年龄在40岁到69岁之间。根据以下糖尿病风险因素对个体进行分层:BMI、糖尿病家族史和全基因组糖尿病多基因风险评分。主要结果指标是整个队列和每个阶层中体重指数每降低 1 kg/m2 患糖尿病的优势比。糖尿病患病率随着体重指数、糖尿病家族史和遗传风险的增加而急剧增加。相反,体重指数和遗传风险类别中减肥带来的预测风险降低惊人地相似。据预测,即使在低风险人群中,体重减轻也会显着降低患糖尿病的几率:例如,体重指数每降低 1 kg/m2,非超重人群的糖尿病几率就会降低 1.37 倍(95% CI 1.12-1.68)无糖尿病家族史的个体(BMI < 25 kg/m2),与有家族史的肥胖个体(BMI ≥ 30 kg/m2)相似(减少 1.21 倍,95% CI 1.13-1.29)。 该分析的一个关键限制是,它所研究的改变BMI的DNA序列多态性代表了个体一生中的累积倾向,因此可能会错误地估计晚年减肥干预措施的风险修正潜力。结论 在人口规模队列中,较低的 BMI 与 BMI、家族史和遗传风险类别的糖尿病风险降低一致相关,这表明所有个体都可以通过减肥来大幅降低糖尿病风险。我们的结果支持对各个糖尿病风险水平的个体广泛部署减肥干预措施。
更新日期:2020-01-14
中文翻译:

英国生物银行体重指数与 2 型糖尿病关联的同质性:孟德尔随机研究。
背景技术降低体重指数(BMI)的生活方式干预是预防2型糖尿病的关键公共卫生策略。虽然减肥干预措施对高风险和糖尿病前期个体显示出明显的益处,但我们的目的是确定同样的益处是否适用于低风险人群。方法和结果 我们对英国生物库中 287,394 名自报的英国白人血统的无关个体进行了一项多层次孟德尔随机化研究,研究 BMI 对糖尿病几率的影响大小,这些个体于 2006 年至 2010 年期间从英国各地招募,当时他们的年龄在40岁到69岁之间。根据以下糖尿病风险因素对个体进行分层:BMI、糖尿病家族史和全基因组糖尿病多基因风险评分。主要结果指标是整个队列和每个阶层中体重指数每降低 1 kg/m2 患糖尿病的优势比。糖尿病患病率随着体重指数、糖尿病家族史和遗传风险的增加而急剧增加。相反,体重指数和遗传风险类别中减肥带来的预测风险降低惊人地相似。据预测,即使在低风险人群中,体重减轻也会显着降低患糖尿病的几率:例如,体重指数每降低 1 kg/m2,非超重人群的糖尿病几率就会降低 1.37 倍(95% CI 1.12-1.68)无糖尿病家族史的个体(BMI < 25 kg/m2),与有家族史的肥胖个体(BMI ≥ 30 kg/m2)相似(减少 1.21 倍,95% CI 1.13-1.29)。 该分析的一个关键限制是,它所研究的改变BMI的DNA序列多态性代表了个体一生中的累积倾向,因此可能会错误地估计晚年减肥干预措施的风险修正潜力。结论 在人口规模队列中,较低的 BMI 与 BMI、家族史和遗传风险类别的糖尿病风险降低一致相关,这表明所有个体都可以通过减肥来大幅降低糖尿病风险。我们的结果支持对各个糖尿病风险水平的个体广泛部署减肥干预措施。











































 京公网安备 11010802027423号
京公网安备 11010802027423号