当前位置:
X-MOL 学术
›
JAMA Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of Long-term Ambient Ozone Exposure With Respiratory Morbidity in Smokers
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamainternmed.2019.5498 Laura M Paulin 1, 2 , Amanda J Gassett 3 , Neil E Alexis 4 , Kipruto Kirwa 3 , Richard E Kanner 5 , Stephen Peters 6 , Jerry A Krishnan 7 , Robert Paine 5 , Mark Dransfield 8 , Prescott G Woodruff 9 , Christopher B Cooper 10 , R Graham Barr 11, 12 , Alejandro P Comellas 13 , Cheryl S Pirozzi 5 , MeiLan Han 14 , Eric A Hoffman 15 , Fernando J Martinez 16 , Han Woo 17 , Roger D Peng 18 , Ashraf Fawzy 17 , Nirupama Putcha 17 , Patrick N Breysse 19, 20 , Joel D Kaufman 3, 21, 22 , Nadia N Hansel 17 ,
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamainternmed.2019.5498 Laura M Paulin 1, 2 , Amanda J Gassett 3 , Neil E Alexis 4 , Kipruto Kirwa 3 , Richard E Kanner 5 , Stephen Peters 6 , Jerry A Krishnan 7 , Robert Paine 5 , Mark Dransfield 8 , Prescott G Woodruff 9 , Christopher B Cooper 10 , R Graham Barr 11, 12 , Alejandro P Comellas 13 , Cheryl S Pirozzi 5 , MeiLan Han 14 , Eric A Hoffman 15 , Fernando J Martinez 16 , Han Woo 17 , Roger D Peng 18 , Ashraf Fawzy 17 , Nirupama Putcha 17 , Patrick N Breysse 19, 20 , Joel D Kaufman 3, 21, 22 , Nadia N Hansel 17 ,
Affiliation
|
Importance
Few studies have investigated the association of long-term ambient ozone exposures with respiratory morbidity among individuals with a heavy smoking history. Objective
To investigate the association of historical ozone exposure with risk of chronic obstructive pulmonary disease (COPD), computed tomography (CT) scan measures of respiratory disease, patient-reported outcomes, disease severity, and exacerbations in smokers with or at risk for COPD. Design, Setting, and Participants
This multicenter cross-sectional study, conducted from November 1, 2010, to July 31, 2018, obtained data from the Air Pollution Study, an ancillary study of SPIROMICS (Subpopulations and Intermediate Outcome Measures in COPD Study). Data analyzed were from participants enrolled at 7 (New York City, New York; Baltimore, Maryland; Los Angeles, California; Ann Arbor, Michigan; San Francisco, California; Salt Lake City, Utah; and Winston-Salem, North Carolina) of the 12 SPIROMICS clinical sites. Included participants had historical ozone exposure data (n = 1874), were either current or former smokers (≥20 pack-years), were with or without COPD, and were aged 40 to 80 years at baseline. Healthy persons with a smoking history of 1 or more pack-years were excluded from the present analysis. Exposures
The 10-year mean historical ambient ozone concentration at participants' residences estimated by cohort-specific spatiotemporal modeling. Main Outcomes and Measures
Spirometry-confirmed COPD, chronic bronchitis diagnosis, CT scan measures (emphysema, air trapping, and airway wall thickness), 6-minute walk test, modified Medical Research Council (mMRC) Dyspnea Scale, COPD Assessment Test (CAT), St. George's Respiratory Questionnaire (SGRQ), postbronchodilator forced expiratory volume in the first second of expiration (FEV1) % predicted, and self-report of exacerbations in the 12 months before SPIROMICS enrollment, adjusted for demographics, smoking, and job exposure. Results
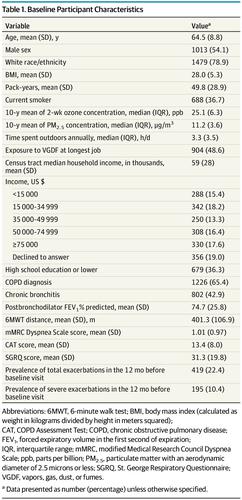
A total of 1874 SPIROMICS participants were analyzed (mean [SD] age, 64.5 [8.8] years; 1479 [78.9%] white; and 1013 [54.1%] male). In adjusted analysis, a 5-ppb (parts per billion) increase in ozone concentration was associated with a greater percentage of emphysema (β = 0.94; 95% CI, 0.25-1.64; P = .007) and percentage of air trapping (β = 1.60; 95% CI, 0.16-3.04; P = .03); worse scores for the mMRC Dyspnea Scale (β = 0.10; 95% CI, 0.03-0.17; P = .008), CAT (β = 0.65; 95% CI, 0.05-1.26; P = .04), and SGRQ (β = 1.47; 95% CI, 0.01-2.93; P = .048); lower FEV1% predicted value (β = -2.50; 95% CI, -4.42 to -0.59; P = .01); and higher odds of any exacerbation (odds ratio [OR], 1.37; 95% CI, 1.12-1.66; P = .002) and severe exacerbation (OR, 1.37; 95% CI, 1.07-1.76; P = .01). No association was found between historical ozone exposure and chronic bronchitis, COPD, airway wall thickness, or 6-minute walk test result. Conclusions and Relevance
This study found that long-term historical ozone exposure was associated with reduced lung function, greater emphysema and air trapping on CT scan, worse patient-reported outcomes, and increased respiratory exacerbations for individuals with a history of heavy smoking. The association between ozone exposure and adverse respiratory outcomes suggests the need for continued reevaluation of ambient pollution standards that are designed to protect the most vulnerable members of the US population.
中文翻译:

长期环境臭氧暴露与吸烟者呼吸道疾病的关联
重要性 很少有研究调查长期环境臭氧暴露与重度吸烟史个体呼吸系统疾病的关联。目的 调查历史臭氧暴露与慢性阻塞性肺病 (COPD) 风险、呼吸系统疾病计算机断层扫描 (CT) 扫描测量、患者报告的结果、疾病严重程度以及患有 COPD 或有患 COPD 风险的吸烟者的恶化之间的关联。设计、设置和参与者 这项多中心横断面研究于 2010 年 11 月 1 日至 2018 年 7 月 31 日进行,从空气污染研究中获取数据,该研究是 SPIROMICS(COPD 研究中的亚群和中间结果测量)的一项辅助研究。分析的数据来自于 7 名参与者(纽约州纽约市;马里兰州巴尔的摩市;加利福尼亚州洛杉矶市;密歇根州安娜堡;加利福尼亚州旧金山;犹他州盐湖城;和 Winston-Salem,北卡罗来纳州)的 12 个 SPIROMICS 临床站点。纳入的参与者有历史臭氧暴露数据(n = 1874),目前或以前吸烟(≥20 包年),有或没有 COPD,基线年龄为 40 至 80 岁。具有 1 年或更多包年吸烟史的健康人被排除在本分析之外。暴露 参与者住宅的 10 年平均历史环境臭氧浓度,通过特定队列时空模型估计。主要结果和测量肺活量测定确认的 COPD、慢性支气管炎诊断、CT 扫描测量(肺气肿、空气滞留和气道壁厚)、6 分钟步行测试、改良的医学研究委员会 (mMRC) 呼吸困难量表、COPD 评估测试 (CAT) , 英石。George 的呼吸问卷 (SGRQ)、呼气后第一秒的支气管扩张剂用力呼气量 (FEV1) % 预测值,以及 SPIROMICS 入组前 12 个月内急性加重的自我报告,根据人口统计学、吸烟和工作接触进行了调整。结果 共分析了 1874 名 SPIROMICS 参与者(平均 [SD] 年龄,64.5 [8.8] 岁;1479 名 [78.9%] 白人;1013 名 [54.1%] 男性)。在调整后的分析中,臭氧浓度增加 5 ppb(十亿分之一)与更大百分比的肺气肿(β = 0.94;95% CI,0.25-1.64;P = .007)和空气滞留百分比(β = 1.60;95% CI,0.16-3.04;P = .03);mMRC 呼吸困难量表 (β = 0.10; 95% CI, 0.03-0.17; P = .008)、CAT (β = 0.65; 95% CI, 0.05-1.26; P = .04) 和 SGRQ (β = 1.47;95% CI,0.01-2.93;P = .048);较低的 FEV1% 预测值(β = -2.50;95% CI,-4.42 至 -0.59;P = .01);任何恶化(比值比 [OR],1.37;95% CI,1.12-1.66;P = .002)和严重恶化(OR,1.37;95% CI,1.07-1.76;P = .01)的几率更高。未发现历史臭氧暴露与慢性支气管炎、COPD、气道壁厚或 6 分钟步行测试结果之间存在关联。结论和相关性 本研究发现,长期历史臭氧暴露与肺功能降低、肺气肿和 CT 扫描中的空气滞留、患者报告的结果更差以及有大量吸烟史的个体的呼吸恶化增加有关。
更新日期:2020-01-01
中文翻译:

长期环境臭氧暴露与吸烟者呼吸道疾病的关联
重要性 很少有研究调查长期环境臭氧暴露与重度吸烟史个体呼吸系统疾病的关联。目的 调查历史臭氧暴露与慢性阻塞性肺病 (COPD) 风险、呼吸系统疾病计算机断层扫描 (CT) 扫描测量、患者报告的结果、疾病严重程度以及患有 COPD 或有患 COPD 风险的吸烟者的恶化之间的关联。设计、设置和参与者 这项多中心横断面研究于 2010 年 11 月 1 日至 2018 年 7 月 31 日进行,从空气污染研究中获取数据,该研究是 SPIROMICS(COPD 研究中的亚群和中间结果测量)的一项辅助研究。分析的数据来自于 7 名参与者(纽约州纽约市;马里兰州巴尔的摩市;加利福尼亚州洛杉矶市;密歇根州安娜堡;加利福尼亚州旧金山;犹他州盐湖城;和 Winston-Salem,北卡罗来纳州)的 12 个 SPIROMICS 临床站点。纳入的参与者有历史臭氧暴露数据(n = 1874),目前或以前吸烟(≥20 包年),有或没有 COPD,基线年龄为 40 至 80 岁。具有 1 年或更多包年吸烟史的健康人被排除在本分析之外。暴露 参与者住宅的 10 年平均历史环境臭氧浓度,通过特定队列时空模型估计。主要结果和测量肺活量测定确认的 COPD、慢性支气管炎诊断、CT 扫描测量(肺气肿、空气滞留和气道壁厚)、6 分钟步行测试、改良的医学研究委员会 (mMRC) 呼吸困难量表、COPD 评估测试 (CAT) , 英石。George 的呼吸问卷 (SGRQ)、呼气后第一秒的支气管扩张剂用力呼气量 (FEV1) % 预测值,以及 SPIROMICS 入组前 12 个月内急性加重的自我报告,根据人口统计学、吸烟和工作接触进行了调整。结果 共分析了 1874 名 SPIROMICS 参与者(平均 [SD] 年龄,64.5 [8.8] 岁;1479 名 [78.9%] 白人;1013 名 [54.1%] 男性)。在调整后的分析中,臭氧浓度增加 5 ppb(十亿分之一)与更大百分比的肺气肿(β = 0.94;95% CI,0.25-1.64;P = .007)和空气滞留百分比(β = 1.60;95% CI,0.16-3.04;P = .03);mMRC 呼吸困难量表 (β = 0.10; 95% CI, 0.03-0.17; P = .008)、CAT (β = 0.65; 95% CI, 0.05-1.26; P = .04) 和 SGRQ (β = 1.47;95% CI,0.01-2.93;P = .048);较低的 FEV1% 预测值(β = -2.50;95% CI,-4.42 至 -0.59;P = .01);任何恶化(比值比 [OR],1.37;95% CI,1.12-1.66;P = .002)和严重恶化(OR,1.37;95% CI,1.07-1.76;P = .01)的几率更高。未发现历史臭氧暴露与慢性支气管炎、COPD、气道壁厚或 6 分钟步行测试结果之间存在关联。结论和相关性 本研究发现,长期历史臭氧暴露与肺功能降低、肺气肿和 CT 扫描中的空气滞留、患者报告的结果更差以及有大量吸烟史的个体的呼吸恶化增加有关。











































 京公网安备 11010802027423号
京公网安备 11010802027423号