Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
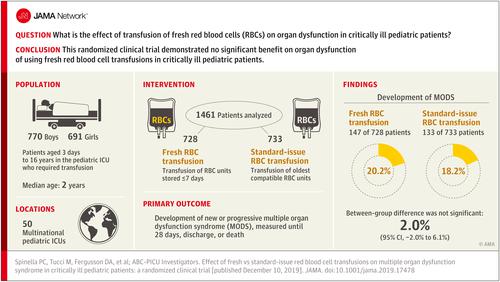
Effect of Fresh vs Standard-issue Red Blood Cell Transfusions on Multiple Organ Dysfunction Syndrome in Critically Ill Pediatric Patients
JAMA ( IF 63.1 ) Pub Date : 2019-12-10 , DOI: 10.1001/jama.2019.17478 Philip C Spinella 1 , Marisa Tucci 2 , Dean A Fergusson 3 , Jacques Lacroix 2 , Paul C Hébert 4 , Stéphane Leteurtre 5 , Kenneth B Schechtman 6 , Allan Doctor 1 , Robert A Berg 7 , Tina Bockelmann 1 , J Jaime Caro 8, 9 , Fabrizio Chiusolo 10 , Lucy Clayton 11 , Jill M Cholette 12 , Gonzalo Garcia Guerra 13, 14 , Cassandra D Josephson 15, 16 , Kusum Menon 17 , Jennifer A Muszynski 18 , Marianne E Nellis 19 , Amrita Sarpal 20 , Stephanie Schafer 1 , Marie E Steiner 21 , Alexis F Turgeon 22 ,
JAMA ( IF 63.1 ) Pub Date : 2019-12-10 , DOI: 10.1001/jama.2019.17478 Philip C Spinella 1 , Marisa Tucci 2 , Dean A Fergusson 3 , Jacques Lacroix 2 , Paul C Hébert 4 , Stéphane Leteurtre 5 , Kenneth B Schechtman 6 , Allan Doctor 1 , Robert A Berg 7 , Tina Bockelmann 1 , J Jaime Caro 8, 9 , Fabrizio Chiusolo 10 , Lucy Clayton 11 , Jill M Cholette 12 , Gonzalo Garcia Guerra 13, 14 , Cassandra D Josephson 15, 16 , Kusum Menon 17 , Jennifer A Muszynski 18 , Marianne E Nellis 19 , Amrita Sarpal 20 , Stephanie Schafer 1 , Marie E Steiner 21 , Alexis F Turgeon 22 ,
Affiliation
|
Importance
The clinical consequences of red blood cell storage age for critically ill pediatric patients have not been examined in a large, randomized clinical trial. Objective
To determine if the transfusion of fresh red blood cells (stored ≤7 days) reduced new or progressive multiple organ dysfunction syndrome compared with the use of standard-issue red blood cells in critically ill children. Design, Setting, and Participants
The Age of Transfused Blood in Critically-Ill Children trial was an international, multicenter, blinded, randomized clinical trial, performed between February 2014 and November 2018 in 50 tertiary care centers. Pediatric patients between the ages of 3 days and 16 years were eligible if the first red blood cell transfusion was administered within 7 days of intensive care unit admission. A total of 15 568 patients were screened, and 13 308 were excluded. Interventions
Patients were randomized to receive either fresh or standard-issue red blood cells. A total of 1538 patients were randomized with 768 patients in the fresh red blood cell group and 770 in the standard-issue group. Main Outcomes and Measures
The primary outcome measure was new or progressive multiple organ dysfunction syndrome, measured for 28 days or to discharge or death. Results
Among 1538 patients who were randomized, 1461 patients (95%) were included in the primary analysis (median age, 1.8 years; 47.3% girls), in which there were 728 patients randomized to the fresh red blood cell group and 733 to the standard-issue group. The median storage duration was 5 days (interquartile range [IQR], 4-6 days) in the fresh group vs 18 days (IQR, 12-25 days) in the standard-issue group (P < .001). There were no significant differences in new or progressive multiple organ dysfunction syndrome between fresh (147 of 728 [20.2%]) and standard-issue red blood cell groups (133 of 732 [18.2%]), with an unadjusted absolute risk difference of 2.0% (95% CI, -2.0% to 6.1%; P = .33). The prevalence of sepsis was 25.8% (160 of 619) in the fresh group and 25.3% (154 of 608) in the standard-issue group. The prevalence of acute respiratory distress syndrome was 6.6% (41 of 619) in the fresh group and 4.8% (29 of 608) in the standard-issue group. Intensive care unit mortality was 4.5% (33 of 728) in the fresh group vs 3.5 % (26 of 732) in the standard-issue group (P = .34). Conclusions and Relevance
Among critically ill pediatric patients, the use of fresh red blood cells did not reduce the incidence of new or progressive multiple organ dysfunction syndrome (including mortality) compared with standard-issue red blood cells. Trial Registration
ClinicalTrials.gov Identifier: NCT01977547.
中文翻译:

新鲜与标准红细胞输注对危重儿科患者多器官功能障碍综合征的影响
重要性尚未在大型随机临床试验中检查危重儿科患者红细胞储存年龄的临床后果。目的 确定与使用标准红细胞相比,输注新鲜红细胞(储存 ≤ 7 天)是否能减少新发或进行性多器官功能障碍综合征。设计、设置和参与者 危重儿童输血年龄试验是一项国际、多中心、盲法、随机临床试验,于 2014 年 2 月至 2018 年 11 月在 50 个三级保健中心进行。如果在重症监护病房入院后 7 天内进行第一次红细胞输注,则年龄在 3 天至 16 岁之间的儿科患者符合条件。共筛查了 15 568 名患者,排除了 13 308 名患者。干预 患者随机接受新鲜或标准红细胞。共有 1538 名患者被随机分组,新鲜红细胞组 768 名,标准分配组 770 名。主要结果和测量 主要结果测量是新的或进行性多器官功能障碍综合征,测量 28 天或出院或死亡。结果 在随机分组的 1538 名患者中,1461 名患者(95%)被纳入主要分析(中位年龄为 1.8 岁;47.3% 为女孩),其中 728 名患者被随机分配至新鲜红细胞组,733 名患者被随机分配至标准问题组。新鲜组的中位储存时间为 5 天(四分位距 [IQR],4-6 天),而新鲜组为 18 天(IQR,12-25 天)在标准问题组(P < .001)。新鲜红细胞组(728 个中的 147 个 [20.2%])和标准红细胞组(732 个中的 133 个 [18.2%])在新发或进行性多器官功能障碍综合征方面没有显着差异,未经调整的绝对风险差异为 2.0 %(95% CI,-2.0% 至 6.1%;P = .33)。新鲜组的败血症患病率为 25.8%(619 人中的 160 人),标准问题组为 25.3%(608 人中的 154 人)。新鲜组的急性呼吸窘迫综合征的患病率为 6.6%(619 人中的 41 人),标准问题组为 4.8%(608 人中的 29 人)。新鲜组的重症监护病房死亡率为 4.5%(728 人中的 33 人),而标准问题组为 3.5%(732 人中的 26 人)(P = .34)。结论及意义 在危重儿科患者中,与标准红细胞相比,使用新鲜红细胞并没有降低新发或进行性多器官功能障碍综合征(包括死亡率)的发生率。试验注册 ClinicalTrials.gov 标识符:NCT01977547。
更新日期:2019-12-10
中文翻译:

新鲜与标准红细胞输注对危重儿科患者多器官功能障碍综合征的影响
重要性尚未在大型随机临床试验中检查危重儿科患者红细胞储存年龄的临床后果。目的 确定与使用标准红细胞相比,输注新鲜红细胞(储存 ≤ 7 天)是否能减少新发或进行性多器官功能障碍综合征。设计、设置和参与者 危重儿童输血年龄试验是一项国际、多中心、盲法、随机临床试验,于 2014 年 2 月至 2018 年 11 月在 50 个三级保健中心进行。如果在重症监护病房入院后 7 天内进行第一次红细胞输注,则年龄在 3 天至 16 岁之间的儿科患者符合条件。共筛查了 15 568 名患者,排除了 13 308 名患者。干预 患者随机接受新鲜或标准红细胞。共有 1538 名患者被随机分组,新鲜红细胞组 768 名,标准分配组 770 名。主要结果和测量 主要结果测量是新的或进行性多器官功能障碍综合征,测量 28 天或出院或死亡。结果 在随机分组的 1538 名患者中,1461 名患者(95%)被纳入主要分析(中位年龄为 1.8 岁;47.3% 为女孩),其中 728 名患者被随机分配至新鲜红细胞组,733 名患者被随机分配至标准问题组。新鲜组的中位储存时间为 5 天(四分位距 [IQR],4-6 天),而新鲜组为 18 天(IQR,12-25 天)在标准问题组(P < .001)。新鲜红细胞组(728 个中的 147 个 [20.2%])和标准红细胞组(732 个中的 133 个 [18.2%])在新发或进行性多器官功能障碍综合征方面没有显着差异,未经调整的绝对风险差异为 2.0 %(95% CI,-2.0% 至 6.1%;P = .33)。新鲜组的败血症患病率为 25.8%(619 人中的 160 人),标准问题组为 25.3%(608 人中的 154 人)。新鲜组的急性呼吸窘迫综合征的患病率为 6.6%(619 人中的 41 人),标准问题组为 4.8%(608 人中的 29 人)。新鲜组的重症监护病房死亡率为 4.5%(728 人中的 33 人),而标准问题组为 3.5%(732 人中的 26 人)(P = .34)。结论及意义 在危重儿科患者中,与标准红细胞相比,使用新鲜红细胞并没有降低新发或进行性多器官功能障碍综合征(包括死亡率)的发生率。试验注册 ClinicalTrials.gov 标识符:NCT01977547。











































 京公网安备 11010802027423号
京公网安备 11010802027423号