当前位置:
X-MOL 学术
›
Am. J. Kidney Dis.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Outcomes From Right Versus Left Deceased-Donor Kidney Transplants: A US National Cohort Study.
American Journal of Kidney Diseases ( IF 9.4 ) Pub Date : 2019-12-05 , DOI: 10.1053/j.ajkd.2019.08.018 Sanjay Kulkarni 1 , Guo Wei 2 , Wei Jiang 3 , Licia A Lopez 4 , Chirag R Parikh 5 , Isaac E Hall 2
American Journal of Kidney Diseases ( IF 9.4 ) Pub Date : 2019-12-05 , DOI: 10.1053/j.ajkd.2019.08.018 Sanjay Kulkarni 1 , Guo Wei 2 , Wei Jiang 3 , Licia A Lopez 4 , Chirag R Parikh 5 , Isaac E Hall 2
Affiliation
|
RATIONALE & OBJECTIVE
There may be important transplant-related differences between right and left kidneys, including logistical/surgical considerations about vessel length for the right compared to the left kidney from the same donor. Because US centers choose between the right and left kidney when their recipient is ranked higher on a "match-run," we sought to determine whether deceased-donor right kidneys have had worse posttransplantation outcomes than left kidneys.
STUDY DESIGN
Paired Organ Procurement and Transplantation Network analysis.
SETTING & PARTICIPANTS
Deceased-donor kidney pairs transplanted during 1990 to 2016.
EXPOSURE
Right versus left kidney controlling for other significant factors.
OUTCOMES
Delayed graft function (DGF), all-cause and death-censored graft failure, and mortality.
ANALYTICAL APPROACH
Multivariable conditional logistic regression for DGF; proportional hazards models (conditional on same donor) for failure/mortality with right kidneys (operationalized as 6-month time-varying coefficients) adjusting for DGF and other confounders.
RESULTS
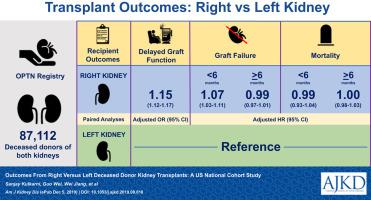
87,112 recipient pairs shared the following donor characteristics: mean age of 41 ± 14 years, 60% males, and 11% with cardiac death. Recipient characteristics were numerically similar by donor kidney side but with some statistical differences given the sample size. Right kidneys had slightly longer cold ischemia time. DGF occurred more often for right kidneys (28% vs 25.8%; P < 0.001; adjusted OR, 1.15 [95% CI, 1.12-1.17]). The adjusted hazard ratio (aHR) for all-cause graft failure with right kidneys within 6 months was 1.07 (95% CI, 1.03-1.11), and was 0.99 (95% CI, 0.97-1.01) thereafter. The aHRs for death-censored graft failure with right kidneys before and after 6 months were 1.11 (95% CI, 1.06-1.16) and 0.96 (95% CI, 0.93-0.99), respectively; the corresonding aHRs for mortality were 0.99 (95% CI, 0.93-1.04) and 1.00 (95% CI, 0.98-1.03), respectively.
LIMITATIONS
Registry data, different transplant eras, reasons for kidney side unavailable.
CONCLUSIONS
There is modest association for transplantation of right kidneys with DGF and graft loss within the first 6 months, which is lost beyond this time point. These findings do not support the use of laterality of deceased-donor kidneys as an important factor in organ acceptance decisions.
中文翻译:

右侧与左侧死者供肾移植的结果:美国国家队列研究。
原理和目标 左右肾之间可能存在重要的移植相关差异,包括与来自同一捐赠者的左肾相比,右侧血管长度的逻辑/手术考虑。由于美国中心在接受者在“比赛运行”中排名较高时会在右肾和左肾之间做出选择,因此我们试图确定已故捐赠者右肾的移植后结果是否比左肾更差。研究设计配对器官采购和移植网络分析。设置和参与者 1990 年至 2016 年期间移植的已故供体肾脏对。暴露 控制其他重要因素的右肾与左肾。结果 移植物功能延迟 (DGF)、全因和死亡审查的移植物失败以及死亡率。分析方法 DGF 的多变量条件逻辑回归;右肾衰竭/死亡的比例风险模型(以同一供体为条件)(作为 6 个月时变系数操作)调整 DGF 和其他混杂因素。结果 87,112 对受者具有以下供体特征:平均年龄为 41 ± 14 岁,60% 为男性,11% 为心脏死亡。供肾侧的受体特征在数值上相似,但鉴于样本量存在一些统计差异。右肾的冷缺血时间稍长。右肾发生 DGF 的频率更高(28% 对 25.8%;P < 0.001;调整后的 OR,1.15 [95% CI,1.12-1.17])。6 个月内右肾全因移植物衰竭的调整风险比 (aHR) 为 1.07(95% CI,1.03-1.11)和 0.99(95% CI,0. 97-1.01)此后。6 个月前后右肾死亡删失移植物衰竭的 aHR 分别为 1.11(95% CI,1.06-1.16)和 0.96(95% CI,0.93-0.99);死亡率的相关 aHR 分别为 0.99(95% CI,0.93-1.04)和 1.00(95% CI,0.98-1.03)。局限性 注册数据、不同移植时代、肾侧原因不可用。结论 右肾移植与前 6 个月内 DGF 和移植物丢失之间存在适度关联,超过该时间点后丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。分别; 死亡率的相关 aHR 分别为 0.99(95% CI,0.93-1.04)和 1.00(95% CI,0.98-1.03)。局限性 注册数据、不同移植时代、肾侧原因不可用。结论 右肾移植与前 6 个月内 DGF 和移植物丢失之间存在适度关联,超过该时间点后丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。分别; 死亡率的相关 aHR 分别为 0.99(95% CI,0.93-1.04)和 1.00(95% CI,0.98-1.03)。局限性 注册数据、不同移植时代、肾侧原因不可用。结论 右肾移植与前 6 个月内 DGF 和移植物丢失之间存在适度关联,超过该时间点后丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。超过这个时间点就会丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。超过这个时间点就会丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。
更新日期:2019-12-05
中文翻译:

右侧与左侧死者供肾移植的结果:美国国家队列研究。
原理和目标 左右肾之间可能存在重要的移植相关差异,包括与来自同一捐赠者的左肾相比,右侧血管长度的逻辑/手术考虑。由于美国中心在接受者在“比赛运行”中排名较高时会在右肾和左肾之间做出选择,因此我们试图确定已故捐赠者右肾的移植后结果是否比左肾更差。研究设计配对器官采购和移植网络分析。设置和参与者 1990 年至 2016 年期间移植的已故供体肾脏对。暴露 控制其他重要因素的右肾与左肾。结果 移植物功能延迟 (DGF)、全因和死亡审查的移植物失败以及死亡率。分析方法 DGF 的多变量条件逻辑回归;右肾衰竭/死亡的比例风险模型(以同一供体为条件)(作为 6 个月时变系数操作)调整 DGF 和其他混杂因素。结果 87,112 对受者具有以下供体特征:平均年龄为 41 ± 14 岁,60% 为男性,11% 为心脏死亡。供肾侧的受体特征在数值上相似,但鉴于样本量存在一些统计差异。右肾的冷缺血时间稍长。右肾发生 DGF 的频率更高(28% 对 25.8%;P < 0.001;调整后的 OR,1.15 [95% CI,1.12-1.17])。6 个月内右肾全因移植物衰竭的调整风险比 (aHR) 为 1.07(95% CI,1.03-1.11)和 0.99(95% CI,0. 97-1.01)此后。6 个月前后右肾死亡删失移植物衰竭的 aHR 分别为 1.11(95% CI,1.06-1.16)和 0.96(95% CI,0.93-0.99);死亡率的相关 aHR 分别为 0.99(95% CI,0.93-1.04)和 1.00(95% CI,0.98-1.03)。局限性 注册数据、不同移植时代、肾侧原因不可用。结论 右肾移植与前 6 个月内 DGF 和移植物丢失之间存在适度关联,超过该时间点后丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。分别; 死亡率的相关 aHR 分别为 0.99(95% CI,0.93-1.04)和 1.00(95% CI,0.98-1.03)。局限性 注册数据、不同移植时代、肾侧原因不可用。结论 右肾移植与前 6 个月内 DGF 和移植物丢失之间存在适度关联,超过该时间点后丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。分别; 死亡率的相关 aHR 分别为 0.99(95% CI,0.93-1.04)和 1.00(95% CI,0.98-1.03)。局限性 注册数据、不同移植时代、肾侧原因不可用。结论 右肾移植与前 6 个月内 DGF 和移植物丢失之间存在适度关联,超过该时间点后丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。超过这个时间点就会丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。超过这个时间点就会丢失。这些发现不支持将已故捐赠者肾脏的偏侧性作为器官接受决定的重要因素。











































 京公网安备 11010802027423号
京公网安备 11010802027423号