当前位置:
X-MOL 学术
›
JAMA Dermatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Evaluation of Patch Test Findings in Patients With Anogenital Dermatitis.
JAMA Dermatology ( IF 11.5 ) Pub Date : 2019-11-27 , DOI: 10.1001/jamadermatol.2019.3844 Erin M Warshaw 1, 2 , Rebecca S Kimyon 1, 3 , Jonathan I Silverberg 4 , Donald V Belsito 5 , Joel G DeKoven 6 , Howard I Maibach 7 , Kathryn A Zug 8 , Amber R Atwater 9 , Toby Mathias 10 , Denis Sasseville 11 , Joseph F Fowler 12 , James G Marks 13 , Margo J Reeder 14 , Vincent A DeLeo 15 , Melanie D Pratt 16 , Matthew J Zirwas 17 , James S Taylor 18 , Anthony F Fransway 19
JAMA Dermatology ( IF 11.5 ) Pub Date : 2019-11-27 , DOI: 10.1001/jamadermatol.2019.3844 Erin M Warshaw 1, 2 , Rebecca S Kimyon 1, 3 , Jonathan I Silverberg 4 , Donald V Belsito 5 , Joel G DeKoven 6 , Howard I Maibach 7 , Kathryn A Zug 8 , Amber R Atwater 9 , Toby Mathias 10 , Denis Sasseville 11 , Joseph F Fowler 12 , James G Marks 13 , Margo J Reeder 14 , Vincent A DeLeo 15 , Melanie D Pratt 16 , Matthew J Zirwas 17 , James S Taylor 18 , Anthony F Fransway 19
Affiliation
|
Importance
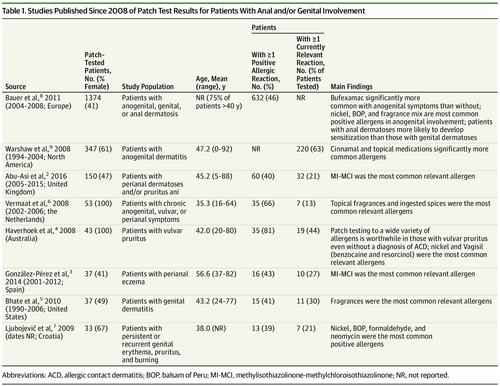
Contact dermatitis in the anogenital area is associated with sleep disturbance and dyspareunia and can profoundly affect quality of life. The literature on anogenital contact dermatitis and culprit allergens is limited. The last large-scale study on common, relevant allergens in patients with anogenital dermatitis was published in 2008.
Objectives
To characterize patients with anogenital dermatitis referred for patch testing by the North American Contact Dermatitis Group, to identify common allergens, and to explore sex-associated differences between anogenital dermatitis and allergens.
Design, Setting, and Participants
A retrospective, cross-sectional analysis was conducted of the North American Contact Dermatitis Group database among 28 481 patients who underwent patch testing from January 1, 2005, to December 31, 2016, at outpatient referral clinics in the United States and Canada.
Exposure
Patch testing for allergens.
Main Outcomes and Measures
Currently relevant allergic patch test reactions in patients with anogenital dermatitis.
Results
Of 28 481 patients tested during the study period, 832 patients (336 men and 496 women; mean [SD] age, 50.1 [26.5] years) had anogenital involvement and 449 patients (177 men and 272 women; mean [SD] age, 49.6 [17.4] years) had anogenital dermatitis only. Compared with those without anogenital involvement, there were significantly more male patients in the group with anogenital dermatitis (177 [39.4%] vs 8857 of 27 649 [32.0%]; relative risk, 1.37; 95% CI, 1.14-1.66; P < .001). In the group with anogenital involvement, female patients were significantly less likely than male patients to have allergic contact dermatitis as a final diagnosis (130 [47.8%] vs 107 [60.5%]; relative risk, 0.78; 95% CI, 0.64-0.94; P = .01), whereas a final diagnosis of other dermatoses (eg, lichen planus, lichen sclerosus, or lichen simplex chronicus) was more frequent for female patients than for male patients (67 [24.6%] vs 28 [15.8%]; relative risk, 1.54; 95% CI, 1.02-2.31; P = .03). Of the 449 patients in the group with anogenital involvement only, 227 (50.6%) had 1 or more relevant reaction with patch testing. Allergens that were statistically significantly more common in patients with anogenital involvement compared with those without anogenital involvement included medicaments such as dibucaine (10 of 250 patients tested [4.0%] vs 32 of 17 494 patients tested [0.2%]; relative risk, 22.74; 95% CI, 11.05-46.78; P < .001) and preservatives such as methylchloroisothiazolinone and methylisothiazolinone (30 of 449 patients tested [6.7%] vs 1143 of 27 599 patients tested [4.1%]; relative risk, 1.61; 95% CI, 1.14-2.41; P = .008). A total of 152 patients met the definition for anogenital allergic contact dermatitis, which is defined as anogenital involvement only, allergic contact dermatitis as the only diagnosis, and 1 or more positive reaction of current clinical relevance.
Conclusions and Relevance
For patients with anogenital involvement only who were referred for patch testing, male patients were more likely to have allergic contact dermatitis, whereas female patients were more likely to have other dermatoses. Common allergens or sources consisted of those likely to contact the anogenital area. For individuals with anogenital involvement suspected of having allergic contact dermatitis, reactions to preservatives, fragrances, medications (particularly topical anesthetics), and topical corticosteroids should be tested.
中文翻译:

肛门生殖器皮炎患者补丁测试结果的评估。
重要性肛门生殖器区域的接触性皮炎与睡眠障碍和性交困难有关,并可能深刻影响生活质量。关于肛门生殖器接触性皮炎和罪魁祸首过敏原的文献有限。关于肛门生殖器皮炎患者常见,相关变应原的最新大规模研究报告于2008年发表。目标是鉴定北美接触性皮炎组转诊进行贴片测试的肛门生殖器皮炎患者的特征,确定常见变应原,并探讨性别-肛门生殖器皮炎和过敏原之间的相关差异。设计,设置和参加者对2005年1月1日至2016年12月期间接受贴片测试的28481例北美接触性皮炎组数据库进行了回顾性横断面分析,在美国和加拿大的门诊转诊诊所。过敏原的暴露斑测试。主要结果和措施当前有关肛门生殖器皮炎患者的过敏性斑贴试验反应。结果在研究期间测试的28481例患者中,有肛门生殖器受累的患者832例(336名男性和496名女性;平均[SD]年龄,50.1 [26.5]岁),以及449例患者(177男性和272名女性;平均[SD]年龄) ,49.6 [17.4]年)仅患有肛门生殖器皮炎。与没有肛门生殖器受累的男性相比,患有肛门生殖器皮炎的男性患者明显更多(177 [39.4%]比8857的27 649 [32.0%];相对危险度为1.37; 95%CI为1.14-1.66; P < .001)。在肛门生殖器受累的人群中,女性患者比男性患者患过敏性接触性皮炎的可能性要低得多(130 [47.8%] vs 107 [60.5%];相对危险度为0.78; 95%CI为0.64-0.94; P = 0.01),女性患者比男性患者对其他皮肤病(例如扁平苔藓,扁平苔藓硬化或慢性扁平苔藓)的最终诊断频率更高(67 [24.6%] vs 28 [15.8%];相对危险度1.54; 95) %CI,1.02-2.31; P = .03)。仅该组中有肛门生殖器受累的449名患者中,有227名(50.6%)进行了斑贴试验后有1例或更多相关反应。具有统计学意义的是,有肛门生殖器受累的变应原比没有肛门生殖器受累的变应原更为显着地多,其中包括地布卡因等药物(测试的250名患者中有10名[4.0%],而测试的17494名患者中有32名[0.2%];相对危险度22.74;95%CI,11.05-46.78;P <.001)和甲基氯异噻唑啉酮和甲基异噻唑啉酮等防腐剂(449名患者中的30名[6.7%],而27599名患者中的1143名[4.1%];相对风险,1.61; 95%CI,1.14-2.41; P =。 008)。共有152名患者达到了肛门生殖器过敏性接触性皮炎的定义,该定义仅定义为肛门生殖器受累,仅诊断为过敏性接触性皮炎,并且当前临床相关性为1个或多个阳性反应。结论和相关性对于仅涉及肛门生殖器受累的患者进行贴片检测,男性患者更可能患有过敏性接触性皮炎,而女性患者则更可能患有其他皮肤病。常见的过敏原或来源包括可能接触生殖器区域的那些。
更新日期:2020-01-08
中文翻译:

肛门生殖器皮炎患者补丁测试结果的评估。
重要性肛门生殖器区域的接触性皮炎与睡眠障碍和性交困难有关,并可能深刻影响生活质量。关于肛门生殖器接触性皮炎和罪魁祸首过敏原的文献有限。关于肛门生殖器皮炎患者常见,相关变应原的最新大规模研究报告于2008年发表。目标是鉴定北美接触性皮炎组转诊进行贴片测试的肛门生殖器皮炎患者的特征,确定常见变应原,并探讨性别-肛门生殖器皮炎和过敏原之间的相关差异。设计,设置和参加者对2005年1月1日至2016年12月期间接受贴片测试的28481例北美接触性皮炎组数据库进行了回顾性横断面分析,在美国和加拿大的门诊转诊诊所。过敏原的暴露斑测试。主要结果和措施当前有关肛门生殖器皮炎患者的过敏性斑贴试验反应。结果在研究期间测试的28481例患者中,有肛门生殖器受累的患者832例(336名男性和496名女性;平均[SD]年龄,50.1 [26.5]岁),以及449例患者(177男性和272名女性;平均[SD]年龄) ,49.6 [17.4]年)仅患有肛门生殖器皮炎。与没有肛门生殖器受累的男性相比,患有肛门生殖器皮炎的男性患者明显更多(177 [39.4%]比8857的27 649 [32.0%];相对危险度为1.37; 95%CI为1.14-1.66; P < .001)。在肛门生殖器受累的人群中,女性患者比男性患者患过敏性接触性皮炎的可能性要低得多(130 [47.8%] vs 107 [60.5%];相对危险度为0.78; 95%CI为0.64-0.94; P = 0.01),女性患者比男性患者对其他皮肤病(例如扁平苔藓,扁平苔藓硬化或慢性扁平苔藓)的最终诊断频率更高(67 [24.6%] vs 28 [15.8%];相对危险度1.54; 95) %CI,1.02-2.31; P = .03)。仅该组中有肛门生殖器受累的449名患者中,有227名(50.6%)进行了斑贴试验后有1例或更多相关反应。具有统计学意义的是,有肛门生殖器受累的变应原比没有肛门生殖器受累的变应原更为显着地多,其中包括地布卡因等药物(测试的250名患者中有10名[4.0%],而测试的17494名患者中有32名[0.2%];相对危险度22.74;95%CI,11.05-46.78;P <.001)和甲基氯异噻唑啉酮和甲基异噻唑啉酮等防腐剂(449名患者中的30名[6.7%],而27599名患者中的1143名[4.1%];相对风险,1.61; 95%CI,1.14-2.41; P =。 008)。共有152名患者达到了肛门生殖器过敏性接触性皮炎的定义,该定义仅定义为肛门生殖器受累,仅诊断为过敏性接触性皮炎,并且当前临床相关性为1个或多个阳性反应。结论和相关性对于仅涉及肛门生殖器受累的患者进行贴片检测,男性患者更可能患有过敏性接触性皮炎,而女性患者则更可能患有其他皮肤病。常见的过敏原或来源包括可能接触生殖器区域的那些。











































 京公网安备 11010802027423号
京公网安备 11010802027423号