当前位置:
X-MOL 学术
›
JAMA Psychiatry
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Comparison of Genetic Liability for Sleep Traits Among Individuals With Bipolar Disorder I or II and Control Participants.
JAMA Psychiatry ( IF 22.5 ) Pub Date : 2019-11-21 , DOI: 10.1001/jamapsychiatry.2019.4079 Katie J S Lewis 1, 2 , Alexander Richards 1 , Robert Karlsson 2 , Ganna Leonenko 1 , Samuel E Jones 3 , Hannah J Jones 4, 5, 6 , Katherine Gordon-Smith 7 , Liz Forty 1 , Valentina Escott-Price 1 , Michael J Owen 1, 8 , Michael N Weedon 3 , Lisa Jones 7 , Nick Craddock 1, 8 , Ian Jones 1, 8 , Mikael Landén 2, 9 , Michael C O'Donovan 1, 8 , Arianna Di Florio 1, 8
JAMA Psychiatry ( IF 22.5 ) Pub Date : 2019-11-21 , DOI: 10.1001/jamapsychiatry.2019.4079 Katie J S Lewis 1, 2 , Alexander Richards 1 , Robert Karlsson 2 , Ganna Leonenko 1 , Samuel E Jones 3 , Hannah J Jones 4, 5, 6 , Katherine Gordon-Smith 7 , Liz Forty 1 , Valentina Escott-Price 1 , Michael J Owen 1, 8 , Michael N Weedon 3 , Lisa Jones 7 , Nick Craddock 1, 8 , Ian Jones 1, 8 , Mikael Landén 2, 9 , Michael C O'Donovan 1, 8 , Arianna Di Florio 1, 8
Affiliation
|
Importance
Insomnia, hypersomnia, and an evening chronotype are common in individuals with bipolar disorder (BD), but whether this reflects shared genetic liability is unclear. Stratifying by BD subtypes could elucidate this association and inform sleep and BD research.
Objective
To assess whether polygenic risk scores (PRSs) for sleep traits are associated with BD subtypes I and II.
Design, Setting, and Participants
This case-control study was conducted in the United Kingdom and Sweden with participants with BD and control participants. Multinomial regression was used to assess whether PRSs for insomnia, daytime sleepiness, sleep duration, and chronotype are associated with BD subtypes compared with control participants. Affected individuals were recruited from the Bipolar Disorder Research Network. Control participants were recruited from the 1958 British Birth Cohort and the UK Blood Service. Analyses were repeated in an independent Swedish sample from August 2018 to July 2019. All participants were of European ancestry.
Exposures
Standardized PRSs derived using alleles from genome-wide association studies of insomnia, sleep duration, daytime sleepiness, and chronotype. These were adjusted for the first 10 population principal components, genotyping platforms, and sex.
Main Outcomes and Measures
Association of PRSs with BD subtypes, determined by semistructured psychiatric interview and case notes.
Results
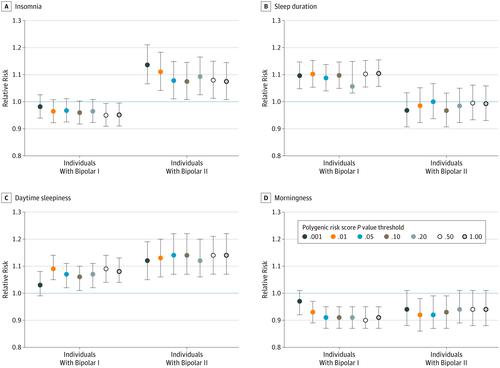
The main analysis included 4672 participants with BD (3132 female participants [67.0%]; 3404 with BD-I [72.9%]) and 5714 control participants (2812 female participants [49.2%]). Insomnia PRS was associated with increased risk of BD-II (relative risk [RR], 1.14 [95% CI, 1.07-1.21]; P = 8.26 × 10-5) but not BD-I (RR, 0.98 [95% CI, 0.94-1.03]; P = .409) relative to control participants. Sleep-duration PRS was associated with BD-I (RR, 1.10 [95% CI, 1.06-1.15]; P = 1.13 × 10-5) but not BD-II (RR, 0.99 [95% CI, 0.93-1.06]; P = .818). Associations between (1) insomnia PRS and BD-II and (2) sleep-duration PRS and BD-I were replicated in the Swedish sample of 4366 individuals with BD (2697 female participants [61.8%]; 2627 with BD-I [60.2%]) and 6091 control participants (3767 female participants [61.8%]). Chronotype and daytime-sleepiness PRS were not associated with BD subtypes.
Conclusions and Relevance
Per this analysis, BD subtypes differ in genetic liability to insomnia and hypersomnia, providing further evidence that the distinction between BD-I and BD-II has genetic validity. This distinction will be crucial in selecting participants for future research on the role of sleep disturbance in BD.
中文翻译:

I型或II型双相情感障碍患者和对照组参与者睡眠特征的遗传责任比较。
躁郁症(BD)患者中普遍存在失眠,失眠和晚型的重要性,但尚不清楚这是否反映了共同的遗传责任。通过BD亚型进行分层可以阐明这种关联,并为睡眠和BD研究提供依据。目的评估睡眠性状的多基因风险评分(PRS)是否与BD亚型I和II相关。设计,设置和参与者这项病例对照研究是在英国和瑞典进行的,有BD参与者和对照参与者。与对照组相比,多项式回归用于评估失眠,白天嗜睡,睡眠时间和表型的PRS是否与BD亚型相关。从双相情感障碍研究网络招募了受影响的个体。控制参与者是从1958年的英国出生队列和英国血液服务局招募的。从2018年8月至2019年7月,在独立的瑞典样本中重复进行了分析。所有参与者均为欧洲血统。暴露使用失眠,睡眠时间,白天嗜睡和表型的全基因组关联研究中的等位基因衍生的标准化PRS。这些已针对前10个人口主要组成部分,基因分型平台和性别进行了调整。由半结构性精神病学访谈和病例记录确定的BD亚型PRS的主要结果和措施协会。结果主要分析包括4672名BD参与者(3132名女性参与者[67.0%]; 3404名BD-I参与者[72.9%])和5714名对照参与者(2812名女性参与者[49.2%])。失眠PRS与BD-II的风险增加相关(相对风险[RR],1.14 [95%CI,1.07-1.21]; P = 8.26×10-5),但与BD-I无关(RR,0.98 [95%CI] ,0.94-1.03]; P = .409)。睡眠持续时间PRS与BD-I(RR,1.10 [95%CI,1.06-1.15]; P = 1.13×10-5)相关,而与BD-II(RR,0.99 [95%CI,0.93-1.06])不相关。 ; P = .818)。(1)失眠PRS和BD-II与(2)睡眠持续时间PRS和BD-I之间的关联在瑞典的4366名BD患者(2697名女性参与者[61.8%]; 2627名BD-I [60.2] %])和6091名对照参与者(3767名女性参与者[61.8%])。慢性亚型和白天嗜睡PRS与BD亚型无关。结论与相关性根据这项分析,BD亚型在失眠和失眠的遗传易感性方面存在差异,提供进一步的证据表明BD-I和BD-II之间的区别具有遗传有效性。这种区别对于选择参与者进行BD睡眠障碍作用的未来研究至关重要。
更新日期:2020-03-05
中文翻译:

I型或II型双相情感障碍患者和对照组参与者睡眠特征的遗传责任比较。
躁郁症(BD)患者中普遍存在失眠,失眠和晚型的重要性,但尚不清楚这是否反映了共同的遗传责任。通过BD亚型进行分层可以阐明这种关联,并为睡眠和BD研究提供依据。目的评估睡眠性状的多基因风险评分(PRS)是否与BD亚型I和II相关。设计,设置和参与者这项病例对照研究是在英国和瑞典进行的,有BD参与者和对照参与者。与对照组相比,多项式回归用于评估失眠,白天嗜睡,睡眠时间和表型的PRS是否与BD亚型相关。从双相情感障碍研究网络招募了受影响的个体。控制参与者是从1958年的英国出生队列和英国血液服务局招募的。从2018年8月至2019年7月,在独立的瑞典样本中重复进行了分析。所有参与者均为欧洲血统。暴露使用失眠,睡眠时间,白天嗜睡和表型的全基因组关联研究中的等位基因衍生的标准化PRS。这些已针对前10个人口主要组成部分,基因分型平台和性别进行了调整。由半结构性精神病学访谈和病例记录确定的BD亚型PRS的主要结果和措施协会。结果主要分析包括4672名BD参与者(3132名女性参与者[67.0%]; 3404名BD-I参与者[72.9%])和5714名对照参与者(2812名女性参与者[49.2%])。失眠PRS与BD-II的风险增加相关(相对风险[RR],1.14 [95%CI,1.07-1.21]; P = 8.26×10-5),但与BD-I无关(RR,0.98 [95%CI] ,0.94-1.03]; P = .409)。睡眠持续时间PRS与BD-I(RR,1.10 [95%CI,1.06-1.15]; P = 1.13×10-5)相关,而与BD-II(RR,0.99 [95%CI,0.93-1.06])不相关。 ; P = .818)。(1)失眠PRS和BD-II与(2)睡眠持续时间PRS和BD-I之间的关联在瑞典的4366名BD患者(2697名女性参与者[61.8%]; 2627名BD-I [60.2] %])和6091名对照参与者(3767名女性参与者[61.8%])。慢性亚型和白天嗜睡PRS与BD亚型无关。结论与相关性根据这项分析,BD亚型在失眠和失眠的遗传易感性方面存在差异,提供进一步的证据表明BD-I和BD-II之间的区别具有遗传有效性。这种区别对于选择参与者进行BD睡眠障碍作用的未来研究至关重要。











































 京公网安备 11010802027423号
京公网安备 11010802027423号