Cellular & Molecular Immunology ( IF 21.8 ) Pub Date : 2019-11-21 , DOI: 10.1038/s41423-019-0325-y Cheng-Hung Lin , Madonna R. Anggelia , Hui-Yun Cheng , Aline Yen Ling Wang , Wen-Yu Chuang , Chih-Hung Lin , W. P. Andrew Lee , Fu-Chan Wei , Gerald Brandacher
|
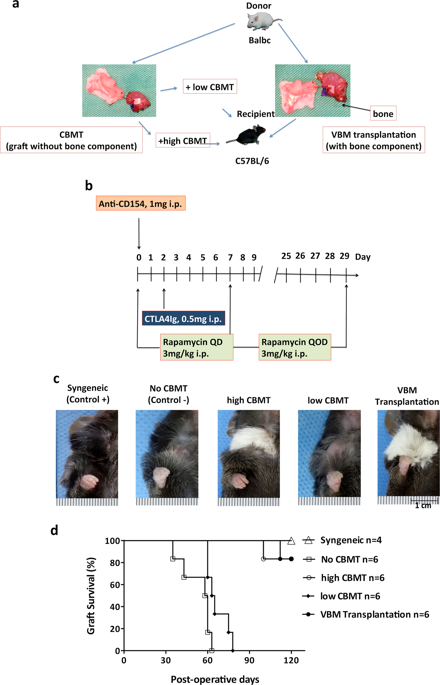
The role of the vascularized bone marrow component as a continuous source of donor-derived hematopoietic stem cells that facilitate tolerance induction of vascularized composite allografts is not completely understood. In this study, vascularized composite tissue allograft transplantation outcomes between recipients receiving either conventional bone marrow transplantation (CBMT) or vascularized bone marrow (VBM) transplantation from Balb/c (H2d) to C57BL/6 (H2b) mice were compared. Either high- or low-dose CBMT (1.5 × 108 or 3 × 107 bone marrow cells, respectively) was applied. In addition, recipients were treated with costimulation blockade (1 mg anti-CD154 and 0.5 mg CTLA4Ig on postoperative days 0 and 2, respectively) and short-term rapamycin (3 mg/kg/day for the first posttransplant week and then every other day for another 3 weeks). Similar to high-dose conventional bone marrow transplantation, 5/6 animals in the vascularized bone marrow group demonstrated long-term allograft survival (>120 days). In contrast, significantly shorter median survival was noted in the low-dose CBMT group (~64 days). Consistently high chimerism levels were observed in the VBM transplantation group. Notably, low levels of circulating CD4+ and CD8+ T cells and a higher ratio of Treg to Teff cells were maintained in VBM transplantation and high-dose CBMT recipients (>30 days) but not in low-dose VBM transplant recipients. Donor-specific hyporesponsiveness was shown in tolerant recipients in vitro. Removal of the vascularized bone marrow component after secondary donor-specific skin transplantation did not affect either primary allograft or secondary skin graft survival.
中文翻译:

移植内血管化骨髓成分在重建移植后的耐受诱导中起关键作用
血管化骨髓成分作为供体源性造血干细胞的连续来源,促进血管化复合同种异体移植物的耐受性诱导,其作用尚不完全清楚。在这项研究中,比较了接受传统骨髓移植 (CBMT) 或血管化骨髓 (VBM) 从 Balb/c (H2d) 移植到 C57BL/6 (H2b) 小鼠的受体之间的血管化复合组织同种异体移植结果。高剂量或低剂量 CBMT(1.5 × 10 8或 3 × 10 7骨髓细胞)。此外,接受者接受共刺激阻断(术后第 0 天和第 2 天分别使用 1 mg 抗 CD154 和 0.5 mg CTLA4Ig)和短期雷帕霉素(移植后第一个周为 3 mg/kg/天,然后每隔一天)再过 3 周)。与高剂量常规骨髓移植相似,血管化骨髓组中有 5/6 的动物表现出长期的同种异体移植存活率(>120 天)。相比之下,低剂量 CBMT 组(~64 天)的中位生存期显着缩短。在 VBM 移植组中观察到始终如一的高嵌合水平。值得注意的是,低水平的循环 CD4 +和 CD8 +在 VBM 移植和高剂量 CBMT 受者(> 30 天)中保持 T 细胞和更高比例的 Treg 与 Teff 细胞,但在低剂量 VBM 移植受者中则不然。在体外耐受受体中显示出供体特异性低反应性。在二次供体特异性皮肤移植后去除血管化的骨髓成分不会影响初次同种异体移植或二次皮肤移植的存活率。











































 京公网安备 11010802027423号
京公网安备 11010802027423号