Experimental & Molecular Medicine ( IF 9.5 ) Pub Date : 2019-11-18 , DOI: 10.1038/s12276-019-0330-3 Hye Sun Lee 1 , Sung Ji Yun 1 , Jung Min Ha 1 , Seo Yeon Jin 1 , Hong Koo Ha 2 , Sang Heon Song 3 , Chi Dae Kim 1 , Sun Sik Bae 1
|
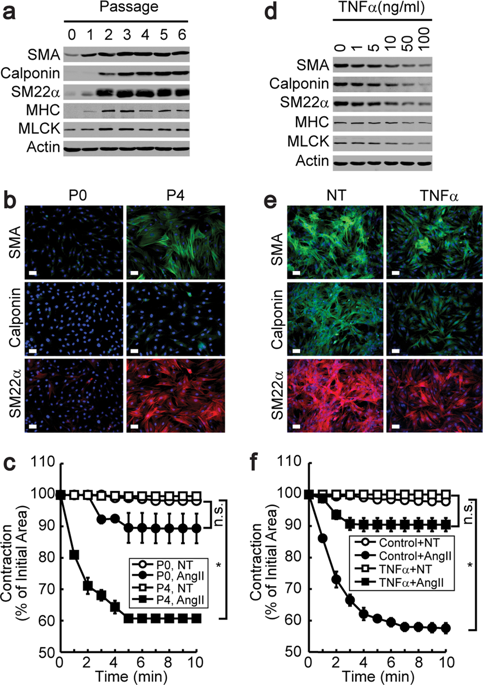
Since chronic inflammation is associated with the pathogenesis of atherosclerosis, inflammatory cytokines might contribute to the phenotypic modulation of vascular smooth muscle cells (VSMCs). Tumor necrosis factor α (TNFα) facilitated the transformation of contractile VSMCs to the synthetic phenotype, as determined by the expression of marker proteins and a collagen gel contraction assay. Western blot analysis and a cyclooxygenase-2 (COX2) promoter assay revealed that TNFα stimulation resulted in the induction of COX2. The overexpression, silencing, or pharmacological inhibition of COX2 significantly affected TNFα-induced phenotypic conversion, and of the tested prostaglandins, only PGD2 significantly induced phenotypic conversion. ERK was significantly activated by PGD2 stimulation, and the pharmacological inhibition of ERK blocked the PGD2-induced phenotypic conversion of VSMCs. However, antagonists or agonists of PGD2 receptors did not affect VSMC conversion. In contrast, spontaneously dehydrated forms of PGD2, such as PGJ2, Δ12-PGJ2, and 15-d-PGJ2, strongly induced phenotypic conversion. A reporter gene assay showed that TNFα, PGD2, and 15-d-PGJ2 significantly activated the peroxisome proliferator-responsive element (PPRE) promoter. In addition, the overexpression or silencing of peroxisome proliferator-activated receptor δ (PPARδ) significantly influenced 15-d-PGJ2-induced phenotypic conversion. Finally, atherosclerotic neointima formation was significantly suppressed in mice lacking TNFα. In addition, mice fed celecoxib exhibited complete inhibition of carotid artery ligation-induced neointima formation. This study shows that PGD2 regulates the phenotypic conversion of VSMCs by generating an endogenous ligand of PPAR, and that this leads to neointima formation in occlusive arterial disease.
中文翻译:

前列腺素 D2 刺激血管平滑肌细胞的表型变化。
由于慢性炎症与动脉粥样硬化的发病机制有关,因此炎性细胞因子可能有助于血管平滑肌细胞 (VSMC) 的表型调节。肿瘤坏死因子 α (TNFα) 促进了收缩性 VSMC 向合成表型的转化,这由标记蛋白的表达和胶原凝胶收缩试验确定。Western印迹分析和环氧合酶2(COX2)启动子测定显示TNFα刺激导致COX2的诱导。COX2 的过表达、沉默或药理学抑制显着影响 TNFα 诱导的表型转换,并且在测试的前列腺素中,只有 PGD 2显着诱导表型转换。ERK 被 PGD 2显着激活刺激,ERK 的药理抑制阻断了 PGD 2诱导的 VSMC 表型转化。然而,PGD 2受体的拮抗剂或激动剂不影响VSMC转化。相反,PGD 2的自发脱水形式,如PGJ 2、Δ 12 -PGJ 2和15-d- PGJ 2,强烈诱导表型转化。报告基因检测显示 TNFα、PGD 2和 15-d-PGJ 2显着激活过氧化物酶体增殖物反应元件 (PPRE) 启动子。此外,过氧化物酶体增殖物激活受体δ (PPARδ) 的过表达或沉默显着影响 15-d-PGJ2-诱导的表型转换。最后,在缺乏 TNFα 的小鼠中,动脉粥样硬化新内膜的形成被显着抑制。此外,喂食塞来昔布的小鼠表现出完全抑制颈动脉结扎诱导的新内膜形成。这项研究表明,PGD 2通过产生 PPAR 的内源性配体来调节 VSMC 的表型转化,这会导致闭塞性动脉疾病中的新内膜形成。











































 京公网安备 11010802027423号
京公网安备 11010802027423号