Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Targeting the IL-1β/EHD1/TUBB3 axis overcomes resistance to EGFR-TKI in NSCLC.
Oncogene ( IF 6.9 ) Pub Date : 2019-11-18 , DOI: 10.1038/s41388-019-1099-5 Jian Huang 1 , Xiuwen Lan 2 , Ting Wang 1 , Hailing Lu 1 , Mengru Cao 1 , Shi Yan 1 , Yue Cui 1 , Dexin Jia 1 , Li Cai 1 , Ying Xing 1
Oncogene ( IF 6.9 ) Pub Date : 2019-11-18 , DOI: 10.1038/s41388-019-1099-5 Jian Huang 1 , Xiuwen Lan 2 , Ting Wang 1 , Hailing Lu 1 , Mengru Cao 1 , Shi Yan 1 , Yue Cui 1 , Dexin Jia 1 , Li Cai 1 , Ying Xing 1
Affiliation
|
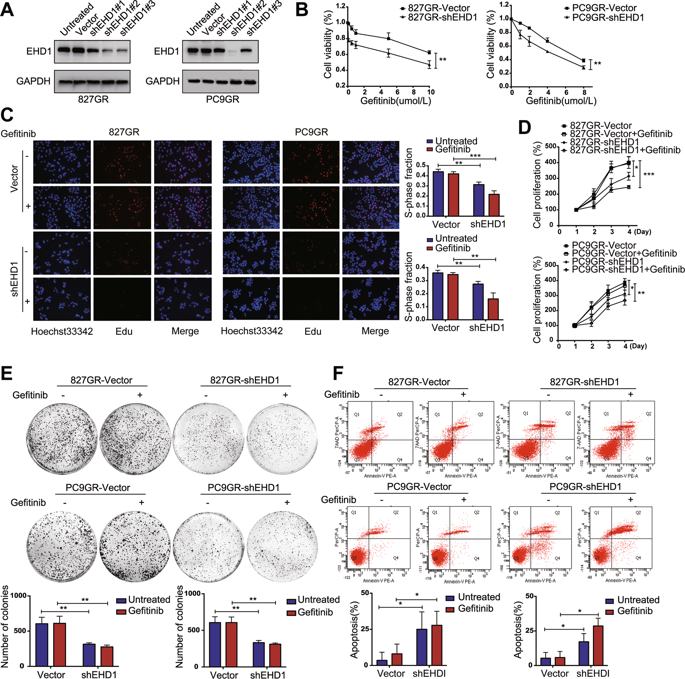
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (EGFR-TKIs) significantly prolong the survival time of non-small-cell lung cancer (NSCLC) patients with EGFR-activating mutations, but resistance develops universally. Activation of the phosphatidyl inositol-3 kinase (PI3K)/AKT signaling pathway and phenotypic alterations in epithelial-mesenchymal transition (EMT) are both mechanisms of acquired resistance to EGFR-TKIs. However, the mechanisms underlying this resistance remain unclear. In this study, EHD1 depletion significantly increased NSCLC cell sensitivity to EGFR-TKI, which was accompanied by EMT reversal. Microarray analysis showed that the PTEN/PI3K/AKT signaling pathway is a crucial pathway regulated by EHD1. Moreover, a PTEN inhibitor abolished EHD1 shRNA regulation of EGFR-TKI sensitivity, EMT, and cancer progression. Mass spectrometry showed that TUBB3 is a novel EHD1-interacting protein. EHD1 modulated microtubule stability by interacting with TUBB3. Furthermore, TUBB3 depletion significantly attenuated EHD1-induced EGFR-TKI resistance and EMT. Bioinformatics analysis revealed that EHD1 is significantly associated with the gene set, "Cellular Response to Interleukin-1β (IL-1β)". As expected, treatment with IL-1β led to increased expression of EHD1, activation of PTEN/PI3K/AKT signaling, and induction of EMT in NSCLC cells. In patient specimens, EHD1 was highly expressed in EGFR-TKI-refractory specimens. EHD1 was positively associated with TUBB3 and IL-1R1 but negatively associated with PTEN. In addition, targeting the IL-1β/EHD1/TUBB3 axis mitigated cancer progression by inhibiting cell proliferation and metastasis and promoting apoptosis. Our study demonstrates the involvement of the IL-1β/EHD1/TUBB3 axis in EGFR-TKI resistance and provides a potential therapeutic approach for treating patients with NSCLC that has acquired EGFR-TKI resistance.
中文翻译:

靶向 IL-1β/EHD1/TUBB3 轴克服了 NSCLC 中对 EGFR-TKI 的耐药性。
表皮生长因子受体 (EGFR) 酪氨酸激酶抑制剂 (EGFR-TKI) 可显着延长具有 EGFR 激活突变的非小细胞肺癌 (NSCLC) 患者的生存时间,但耐药性普遍存在。磷脂酰肌醇 3 激酶 (PI3K)/AKT 信号通路的激活和上皮间质转化 (EMT) 的表型改变都是对 EGFR-TKI 获得性耐药的机制。然而,这种抗性背后的机制仍不清楚。在这项研究中,EHD1 耗竭显着增加了 NSCLC 细胞对 EGFR-TKI 的敏感性,同时伴随着 EMT 逆转。微阵列分析表明PTEN/PI3K/AKT信号通路是EHD1调控的关键通路。此外,一种 PTEN 抑制剂消除了 EHD1 shRNA 对 EGFR-TKI 敏感性、EMT 和癌症进展的调节。质谱分析表明TUBB3 是一种新型的EHD1 相互作用蛋白。EHD1 通过与 TUBB3 相互作用调节微管稳定性。此外,TUBB3 耗竭显着减弱了 EHD1 诱导的 EGFR-TKI 抗性和 EMT。生物信息学分析显示,EHD1 与基因组“细胞对白介素 1β (IL-1β) 的反应”显着相关。正如预期的那样,用 IL-1β 治疗导致 EHD1 的表达增加、PTEN/PI3K/AKT 信号传导的激活和 EMT 在 NSCLC 细胞中的诱导。在患者标本中,EHD1 在 EGFR-TKI 难治性标本中高度表达。EHD1 与 TUBB3 和 IL-1R1 呈正相关,但与 PTEN 呈负相关。此外,靶向 IL-1β/EHD1/TUBB3 轴通过抑制细胞增殖和转移以及促进细胞凋亡来减缓癌症进展。
更新日期:2019-11-18
中文翻译:

靶向 IL-1β/EHD1/TUBB3 轴克服了 NSCLC 中对 EGFR-TKI 的耐药性。
表皮生长因子受体 (EGFR) 酪氨酸激酶抑制剂 (EGFR-TKI) 可显着延长具有 EGFR 激活突变的非小细胞肺癌 (NSCLC) 患者的生存时间,但耐药性普遍存在。磷脂酰肌醇 3 激酶 (PI3K)/AKT 信号通路的激活和上皮间质转化 (EMT) 的表型改变都是对 EGFR-TKI 获得性耐药的机制。然而,这种抗性背后的机制仍不清楚。在这项研究中,EHD1 耗竭显着增加了 NSCLC 细胞对 EGFR-TKI 的敏感性,同时伴随着 EMT 逆转。微阵列分析表明PTEN/PI3K/AKT信号通路是EHD1调控的关键通路。此外,一种 PTEN 抑制剂消除了 EHD1 shRNA 对 EGFR-TKI 敏感性、EMT 和癌症进展的调节。质谱分析表明TUBB3 是一种新型的EHD1 相互作用蛋白。EHD1 通过与 TUBB3 相互作用调节微管稳定性。此外,TUBB3 耗竭显着减弱了 EHD1 诱导的 EGFR-TKI 抗性和 EMT。生物信息学分析显示,EHD1 与基因组“细胞对白介素 1β (IL-1β) 的反应”显着相关。正如预期的那样,用 IL-1β 治疗导致 EHD1 的表达增加、PTEN/PI3K/AKT 信号传导的激活和 EMT 在 NSCLC 细胞中的诱导。在患者标本中,EHD1 在 EGFR-TKI 难治性标本中高度表达。EHD1 与 TUBB3 和 IL-1R1 呈正相关,但与 PTEN 呈负相关。此外,靶向 IL-1β/EHD1/TUBB3 轴通过抑制细胞增殖和转移以及促进细胞凋亡来减缓癌症进展。











































 京公网安备 11010802027423号
京公网安备 11010802027423号