当前位置:
X-MOL 学术
›
JAMA Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Effect of Internet-Distributed HIV Self-tests on HIV Diagnosis and Behavioral Outcomes in Men Who Have Sex With Men
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamainternmed.2019.5222 Robin J MacGowan 1 , Pollyanna R Chavez 1 , Craig B Borkowf 1 , S Michele Owen 1 , David W Purcell 1 , Jonathan H Mermin 1 , Patrick S Sullivan 2 ,
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamainternmed.2019.5222 Robin J MacGowan 1 , Pollyanna R Chavez 1 , Craig B Borkowf 1 , S Michele Owen 1 , David W Purcell 1 , Jonathan H Mermin 1 , Patrick S Sullivan 2 ,
Affiliation
|
Importance
Undiagnosed HIV infection results in delayed access to treatment and increased transmission. Self-tests for HIV may increase awareness of infection among men who have sex with men (MSM). Objective
To evaluate the effect of providing HIV self-tests on frequency of testing, diagnoses of HIV infection, and sexual risk behaviors. Design, Setting, and Participants
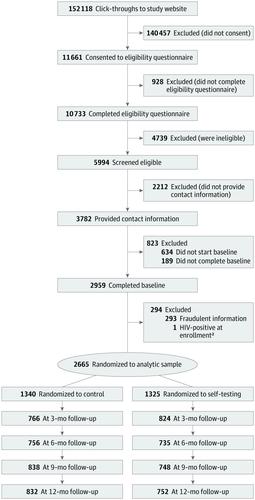
This 12-month longitudinal, 2-group randomized clinical trial recruited MSM through online banner advertisements from March through August 2015. Those recruited were at least 18 years of age, reported engaging in anal sex with men in the past year, never tested positive for HIV, and were US residents with mailing addresses. Participants completed quarterly online surveys. Telephone call notes and laboratory test results were included in the analysis, which was completed from August 2017 through December 2018. Interventions
All participants had access to online web-based HIV testing resources and telephone counseling on request. Participants were randomized in a 1:1 ratio to the control group or a self-testing (ST) group, which received 4 HIV self-tests after completing the baseline survey with the option to replenish self-tests after completing quarterly surveys. At study completion, all participants were offered 2 self-tests and 1 dried blood spot collection kit. Main Outcomes and Measures
Primary outcomes were HIV testing frequency (tested ≥3 times during the trial) and number of newly identified HIV infections among participants in both groups and social network members who used the study HIV self-tests. Secondary outcomes included sex behaviors (eg, anal sex, serosorting). Results
Of 2665 participants, the mean (SD) age was 30 (9.6) years, 1540 (57.8%) were white, and 443 (16.6%) had never tested for HIV before enrollment. Retention rates at each time point were more than 54%, and 1991 (74.7%) participants initiated 1 or more follow-up surveys. More ST participants reported testing 3 or more times during the trial than control participants (777 of 1014 [76.6%] vs 215 of 977 [22.0%]; P < .01). The cumulative number of newly identified infections during the trial was twice as high in the ST participants as the control participants (25 of 1325 [1.9%] vs 11 of 1340 [0.8%]; P = .02), with the largest difference in HIV infections identified in the first 3 months (12 of 1325 [0.9%] vs 2 of 1340 [0.1%]; P < .01). The ST participants reported 34 newly identified infections among social network members who used the self-tests. Conclusions and Relevance
Distribution of HIV self-tests provides a worthwhile mechanism to increase awareness of HIV infection and prevent transmission among MSM. Trial Registration
ClinicalTrials.gov identifier: NCT02067039.
中文翻译:

互联网分发的 HIV 自我检测对男男性行为者 HIV 诊断和行为结果的影响
重要性 未确诊的 HIV 感染会导致治疗延迟和传播增加。HIV 自我检测可能会提高男男性行为者 (MSM) 对感染的认识。目的 评估提供 HIV 自我检测对检测频率、HIV 感染诊断和性风险行为的影响。设计、设置和参与者 这项为期 12 个月的纵向、2 组随机临床试验于 2015 年 3 月至 8 月通过在线横幅广告招募 MSM。招募者至少 18 岁,报告过去与男性发生过肛交年,从未检测出 HIV 阳性,并且是有邮寄地址的美国居民。参与者完成了季度在线调查。分析中包括电话记录和实验室测试结果,2017 年 8 月至 2018 年 12 月完成。 干预 所有参与者都可以访问基于网络的在线 HIV 检测资源并应要求提供电话咨询。参与者以 1:1 的比例随机分配到对照组或自我检测 (ST) 组,在完成基线调查后接受 4 次 HIV 自我检测,并可选择在完成季度调查后补充自我检测。研究完成后,所有参与者都接受了 2 次自测和 1 次干血斑采集套件。主要结果和措施 主要结果是 HIV 检测频率(试验期间检测 ≥ 3 次)和使用研究 HIV 自我检测的两组参与者和社交网络成员中新发现的 HIV 感染人数。次要结果包括性行为(例如,肛交、血清分选)。结果 在 2665 名参与者中,平均 (SD) 年龄为 30 (9.6) 岁,1540 (57.8%) 名白人,443 (16.6%) 名参与者在入组前从未检测过 HIV。每个时间点的保留率都超过 54%,1991 名(74.7%)参与者发起了 1 次或多次随访调查。与对照组相比,更多的 ST 参与者报告在试验期间进行了 3 次或更多次测试(1014 人中有 777 人 [76.6%] vs 977 人中有 215 人 [22.0%];P < .01)。试验期间新发现感染的累积数量在 ST 参与者中是对照组参与者的两倍(1325 人中的 25 人 [1.9%] vs 1340 人中的 11 人 [0.8%];P = .02),差异最大的是在前 3 个月内发现 HIV 感染(1325 例中的 12 例 [0.9%] vs 1340 例中的 2 例 [0.1%];P < .01)。ST 参与者报告了在使用自测的社交网络成员中新发现的 34 例感染。结论和相关性 HIV 自我检测的分布为提高对 HIV 感染的认识和预防 MSM 之间的传播提供了一种有价值的机制。试验注册 ClinicalTrials.gov 标识符:NCT02067039。
更新日期:2020-01-01
中文翻译:

互联网分发的 HIV 自我检测对男男性行为者 HIV 诊断和行为结果的影响
重要性 未确诊的 HIV 感染会导致治疗延迟和传播增加。HIV 自我检测可能会提高男男性行为者 (MSM) 对感染的认识。目的 评估提供 HIV 自我检测对检测频率、HIV 感染诊断和性风险行为的影响。设计、设置和参与者 这项为期 12 个月的纵向、2 组随机临床试验于 2015 年 3 月至 8 月通过在线横幅广告招募 MSM。招募者至少 18 岁,报告过去与男性发生过肛交年,从未检测出 HIV 阳性,并且是有邮寄地址的美国居民。参与者完成了季度在线调查。分析中包括电话记录和实验室测试结果,2017 年 8 月至 2018 年 12 月完成。 干预 所有参与者都可以访问基于网络的在线 HIV 检测资源并应要求提供电话咨询。参与者以 1:1 的比例随机分配到对照组或自我检测 (ST) 组,在完成基线调查后接受 4 次 HIV 自我检测,并可选择在完成季度调查后补充自我检测。研究完成后,所有参与者都接受了 2 次自测和 1 次干血斑采集套件。主要结果和措施 主要结果是 HIV 检测频率(试验期间检测 ≥ 3 次)和使用研究 HIV 自我检测的两组参与者和社交网络成员中新发现的 HIV 感染人数。次要结果包括性行为(例如,肛交、血清分选)。结果 在 2665 名参与者中,平均 (SD) 年龄为 30 (9.6) 岁,1540 (57.8%) 名白人,443 (16.6%) 名参与者在入组前从未检测过 HIV。每个时间点的保留率都超过 54%,1991 名(74.7%)参与者发起了 1 次或多次随访调查。与对照组相比,更多的 ST 参与者报告在试验期间进行了 3 次或更多次测试(1014 人中有 777 人 [76.6%] vs 977 人中有 215 人 [22.0%];P < .01)。试验期间新发现感染的累积数量在 ST 参与者中是对照组参与者的两倍(1325 人中的 25 人 [1.9%] vs 1340 人中的 11 人 [0.8%];P = .02),差异最大的是在前 3 个月内发现 HIV 感染(1325 例中的 12 例 [0.9%] vs 1340 例中的 2 例 [0.1%];P < .01)。ST 参与者报告了在使用自测的社交网络成员中新发现的 34 例感染。结论和相关性 HIV 自我检测的分布为提高对 HIV 感染的认识和预防 MSM 之间的传播提供了一种有价值的机制。试验注册 ClinicalTrials.gov 标识符:NCT02067039。











































 京公网安备 11010802027423号
京公网安备 11010802027423号