当前位置:
X-MOL 学术
›
Nat. Rev. Dis. Primers
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Bronchopulmonary dysplasia.
Nature Reviews Disease Primers ( IF 81.5 ) Pub Date : 2019-11-14 , DOI: 10.1038/s41572-019-0127-7 Bernard Thébaud 1, 2 , Kara N Goss 3 , Matthew Laughon 4 , Jeffrey A Whitsett 5 , Steven H Abman 6 , Robin H Steinhorn 7 , Judy L Aschner 8, 9 , Peter G Davis 10 , Sharon A McGrath-Morrow 11 , Roger F Soll 12 , Alan H Jobe 5
Nature Reviews Disease Primers ( IF 81.5 ) Pub Date : 2019-11-14 , DOI: 10.1038/s41572-019-0127-7 Bernard Thébaud 1, 2 , Kara N Goss 3 , Matthew Laughon 4 , Jeffrey A Whitsett 5 , Steven H Abman 6 , Robin H Steinhorn 7 , Judy L Aschner 8, 9 , Peter G Davis 10 , Sharon A McGrath-Morrow 11 , Roger F Soll 12 , Alan H Jobe 5
Affiliation
|
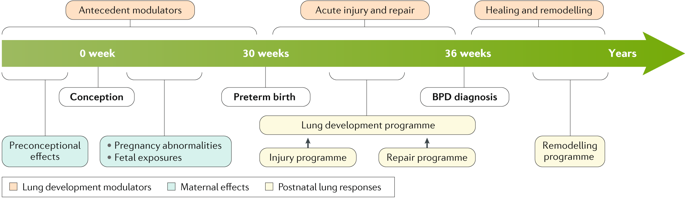
In the absence of effective interventions to prevent preterm births, improved survival of infants who are born at the biological limits of viability has relied on advances in perinatal care over the past 50 years. Except for extremely preterm infants with suboptimal perinatal care or major antenatal events that cause severe respiratory failure at birth, most extremely preterm infants now survive, but they often develop chronic lung dysfunction termed bronchopulmonary dysplasia (BPD; also known as chronic lung disease). Despite major efforts to minimize injurious but often life-saving postnatal interventions (such as oxygen, mechanical ventilation and corticosteroids), BPD remains the most frequent complication of extreme preterm birth. BPD is now recognized as the result of an aberrant reparative response to both antenatal injury and repetitive postnatal injury to the developing lungs. Consequently, lung development is markedly impaired, which leads to persistent airway and pulmonary vascular disease that can affect adult lung function. Greater insights into the pathobiology of BPD will provide a better understanding of disease mechanisms and lung repair and regeneration, which will enable the discovery of novel therapeutic targets. In parallel, clinical and translational studies that improve the classification of disease phenotypes and enable early identification of at-risk preterm infants should improve trial design and individualized care to enhance outcomes in preterm infants.
中文翻译:

支气管肺发育不良。
在缺乏预防早产的有效干预措施的情况下,过去50年来,依靠生存力的生物学极限而出生的婴儿的更好的生存依赖于围产期护理的进步。除了极不佳的围产期护理或严重的产前事件导致出生时出现严重呼吸衰竭的极早产儿,大多数极早产儿现在都可以生存,但是他们经常发展为称为支气管肺不典型增生(BPD;也称为慢性肺病)的慢性肺功能不全。尽管尽了最大的努力来减少伤害性的但通常可以挽救生命的产后干预措施(例如氧气,机械通气和皮质类固醇),但BPD仍然是极端早产的最常见并发症。现在,人们公认BPD是对产前损伤和发育中肺部重复性产后损伤的异常修复反应的结果。因此,肺部发育明显受损,导致持续的气道和肺血管疾病,可能影响成年肺功能。对BPD病理生物学的深入了解将提供对疾病机制以及肺修复和再生的更好理解,这将使发现新的治疗靶标成为可能。同时,改善疾病表型分类并能及早识别高危早产儿的临床和转化研究应改善试验设计和个性化护理,以提高早产儿的预后。这会导致持续的气道和肺血管疾病,从而影响成人的肺功能。对BPD病理生物学的深入了解将提供对疾病机制以及肺修复和再生的更好理解,这将使发现新的治疗靶标成为可能。同时,改善疾病表型分类并能及早识别高危早产儿的临床和转化研究应改善试验设计和个性化护理,以提高早产儿的预后。这会导致持续的气道和肺血管疾病,从而影响成人的肺功能。对BPD病理生物学的深入了解将提供对疾病机制以及肺修复和再生的更好理解,这将使发现新的治疗靶标成为可能。同时,改善疾病表型分类并能及早识别高危早产儿的临床和转化研究应改善试验设计和个性化护理,以提高早产儿的预后。
更新日期:2019-11-14
中文翻译:

支气管肺发育不良。
在缺乏预防早产的有效干预措施的情况下,过去50年来,依靠生存力的生物学极限而出生的婴儿的更好的生存依赖于围产期护理的进步。除了极不佳的围产期护理或严重的产前事件导致出生时出现严重呼吸衰竭的极早产儿,大多数极早产儿现在都可以生存,但是他们经常发展为称为支气管肺不典型增生(BPD;也称为慢性肺病)的慢性肺功能不全。尽管尽了最大的努力来减少伤害性的但通常可以挽救生命的产后干预措施(例如氧气,机械通气和皮质类固醇),但BPD仍然是极端早产的最常见并发症。现在,人们公认BPD是对产前损伤和发育中肺部重复性产后损伤的异常修复反应的结果。因此,肺部发育明显受损,导致持续的气道和肺血管疾病,可能影响成年肺功能。对BPD病理生物学的深入了解将提供对疾病机制以及肺修复和再生的更好理解,这将使发现新的治疗靶标成为可能。同时,改善疾病表型分类并能及早识别高危早产儿的临床和转化研究应改善试验设计和个性化护理,以提高早产儿的预后。这会导致持续的气道和肺血管疾病,从而影响成人的肺功能。对BPD病理生物学的深入了解将提供对疾病机制以及肺修复和再生的更好理解,这将使发现新的治疗靶标成为可能。同时,改善疾病表型分类并能及早识别高危早产儿的临床和转化研究应改善试验设计和个性化护理,以提高早产儿的预后。这会导致持续的气道和肺血管疾病,从而影响成人的肺功能。对BPD病理生物学的深入了解将提供对疾病机制以及肺修复和再生的更好理解,这将使发现新的治疗靶标成为可能。同时,改善疾病表型分类并能及早识别高危早产儿的临床和转化研究应改善试验设计和个性化护理,以提高早产儿的预后。



























 京公网安备 11010802027423号
京公网安备 11010802027423号