Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Associations of maternal quitting, reducing, and continuing smoking during pregnancy with longitudinal fetal growth: Findings from Mendelian randomization and parental negative control studies.
PLOS Medicine ( IF 10.5 ) Pub Date : 2019-11-13 , DOI: 10.1371/journal.pmed.1002972 Judith S Brand 1, 2, 3 , Romy Gaillard 4, 5 , Jane West 2, 3, 6 , Rosemary R C McEachan 6 , John Wright 6 , Ellis Voerman 4, 5 , Janine F Felix 4, 5, 7 , Kate Tilling 2, 3 , Deborah A Lawlor 2, 3, 8
PLOS Medicine ( IF 10.5 ) Pub Date : 2019-11-13 , DOI: 10.1371/journal.pmed.1002972 Judith S Brand 1, 2, 3 , Romy Gaillard 4, 5 , Jane West 2, 3, 6 , Rosemary R C McEachan 6 , John Wright 6 , Ellis Voerman 4, 5 , Janine F Felix 4, 5, 7 , Kate Tilling 2, 3 , Deborah A Lawlor 2, 3, 8
Affiliation
|
BACKGROUND
Maternal smoking during pregnancy is an established risk factor for low infant birth weight, but evidence on critical exposure windows and timing of fetal growth restriction is limited. Here we investigate the associations of maternal quitting, reducing, and continuing smoking during pregnancy with longitudinal fetal growth by triangulating evidence from 3 analytical approaches to strengthen causal inference.
METHODS AND FINDINGS
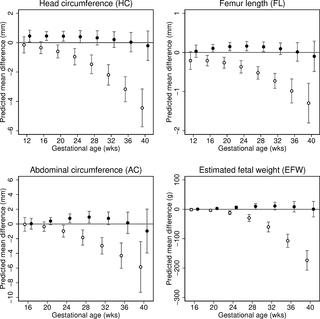
We analysed data from 8,621 European liveborn singletons in 2 population-based pregnancy cohorts (the Generation R Study, the Netherlands 2002-2006 [n = 4,682]) and the Born in Bradford study, United Kingdom 2007-2010 [n = 3,939]) with fetal ultrasound and birth anthropometric measures, parental smoking during pregnancy, and maternal genetic data. Associations with trajectories of estimated fetal weight (EFW) and individual fetal parameters (head circumference, femur length [FL], and abdominal circumference [AC]) from 12-16 to 40 weeks' gestation were analysed using multilevel fractional polynomial models. We compared results from (1) confounder-adjusted multivariable analyses, (2) a Mendelian randomization (MR) analysis using maternal rs1051730 genotype as an instrument for smoking quantity and ease of quitting, and (3) a negative control analysis comparing maternal and mother's partner's smoking associations. In multivariable analyses, women who continued smoking during pregnancy had a smaller fetal size than non-smokers from early gestation (16-20 weeks) through to birth (p-value for each parameter < 0.001). Fetal size reductions in continuing smokers followed a dose-dependent pattern (compared to non-smokers, difference in mean EFW [95% CI] at 40 weeks' gestation was -144 g [-182 to -106], -215 g [-248 to -182], and -290 g [-334 to -247] for light, moderate, and heavy smoking, respectively). Overall, fetal size reductions were most pronounced for FL. The fetal growth trajectory in women who quit smoking in early pregnancy was similar to that of non-smokers, except for a shorter FL and greater AC around 36-40 weeks' gestation. In MR analyses, each genetically determined 1-cigarette-per-day increase was associated with a smaller EFW from 20 weeks' gestation to birth in smokers (p = 0.01, difference in mean EFW at 40 weeks = -45 g [95% CI -81 to -10]) and a greater EFW from 32 weeks' gestation onwards in non-smokers (p = 0.03, difference in mean EFW at 40 weeks = 26 g [95% CI 5 to 47]). There was no evidence that partner smoking was associated with fetal growth. Study limitations include measurement error due to maternal self-report of smoking and the modest sample size for MR analyses resulting in unconfounded estimates being less precise. The apparent positive association of the genetic instrument with fetal growth in non-smokers suggests that genetic pleiotropy may have masked a stronger association in smokers.
CONCLUSIONS
A consistent linear dose-dependent association of maternal smoking with fetal growth was observed from the early second trimester onwards, while no major growth deficit was found in women who quit smoking early in pregnancy except for a shorter FL during late gestation. These findings reinforce the importance of smoking cessation advice in preconception and antenatal care and show that smoking reduction can lower the risk of impaired fetal growth in women who struggle to quit.
中文翻译:

怀孕期间母亲戒烟、减少和继续吸烟与胎儿纵向生长的关联:孟德尔随机化和父母阴性对照研究的结果。
背景 怀孕期间母亲吸烟是婴儿出生体重过低的既定风险因素,但有关关键暴露窗口和胎儿生长受限时间的证据有限。在这里,我们通过三角分析来自 3 种分析方法的证据来加强因果推理,调查孕期母亲戒烟、减少和继续吸烟与胎儿纵向生长的关系。方法和结果 我们分析了 2 个基于人群的妊娠队列(荷兰 2002-2006 年 R 代研究 [n = 4,682])和英国 2007-2010 年出生于布拉德福德的研究 [n = 3,939])与胎儿超声和出生人体测量、怀孕期间父母吸烟和母体遗传数据。使用多级分数多项式模型分析了从妊娠 12-16 到 40 周与估计胎儿体重 (EFW) 和个体胎儿参数(头围、股骨长度 [FL] 和腹围 [AC])轨迹的关联。我们比较了 (1) 混杂因素调整多变量分析的结果,(2) 使用母体 rs1051730 基因型作为衡量吸烟量和戒烟难易程度的孟德尔随机化 (MR) 分析,以及 (3) 比较母体和母亲的阴性对照分析的结果。伴侣的吸烟协会。在多变量分析中,从妊娠早期(16-20 周)到出生(每个参数的 p 值 < 0.001),在怀孕期间继续吸烟的女性的胎儿大小比不吸烟的女性小。持续吸烟者的胎儿尺寸减小遵循剂量依赖性模式(与非吸烟者相比,妊娠 40 周时平均 EFW [95% CI] 的差异为 -144 g [-182 至 -106],-215 g [- 248 到 -182] 和 -290 g [-334 到 -247] 分别用于轻度、中度和重度吸烟)。总体而言,FL 的胎儿体积减小最为明显。妊娠早期戒烟妇女的胎儿生长轨迹与非吸烟者相似,只是在妊娠 36-40 周左右,FL 较短,AC 较大。在 MR 分析中,基因决定的每天增加 1 支香烟与吸烟者从妊娠 20 周到出生的 EFW 较小相关(p = 0.01,40 周时平均 EFW 的差异 = -45 g [95% CI -81 到 -10]),并且从妊娠 32 周开始,非吸烟者的 EFW 更高(p = 0.03,40 周时平均 EFW 的差异 = 26 g [95% CI 5 至 47])。没有证据表明伴侣吸烟与胎儿生长有关。研究限制包括由于母亲自我报告吸烟导致的测量误差和 MR 分析的适度样本量导致无混淆的估计不太精确。遗传工具与非吸烟者胎儿生长的明显正相关表明遗传多效性可能掩盖了吸烟者更强的关联。结论 从妊娠中期早期开始观察到母亲吸烟与胎儿生长呈一致的线性剂量依赖性关联,而在妊娠早期戒烟的女性中没有发现主要的生长缺陷,除了妊娠晚期的 FL 较短。
更新日期:2019-12-03
中文翻译:

怀孕期间母亲戒烟、减少和继续吸烟与胎儿纵向生长的关联:孟德尔随机化和父母阴性对照研究的结果。
背景 怀孕期间母亲吸烟是婴儿出生体重过低的既定风险因素,但有关关键暴露窗口和胎儿生长受限时间的证据有限。在这里,我们通过三角分析来自 3 种分析方法的证据来加强因果推理,调查孕期母亲戒烟、减少和继续吸烟与胎儿纵向生长的关系。方法和结果 我们分析了 2 个基于人群的妊娠队列(荷兰 2002-2006 年 R 代研究 [n = 4,682])和英国 2007-2010 年出生于布拉德福德的研究 [n = 3,939])与胎儿超声和出生人体测量、怀孕期间父母吸烟和母体遗传数据。使用多级分数多项式模型分析了从妊娠 12-16 到 40 周与估计胎儿体重 (EFW) 和个体胎儿参数(头围、股骨长度 [FL] 和腹围 [AC])轨迹的关联。我们比较了 (1) 混杂因素调整多变量分析的结果,(2) 使用母体 rs1051730 基因型作为衡量吸烟量和戒烟难易程度的孟德尔随机化 (MR) 分析,以及 (3) 比较母体和母亲的阴性对照分析的结果。伴侣的吸烟协会。在多变量分析中,从妊娠早期(16-20 周)到出生(每个参数的 p 值 < 0.001),在怀孕期间继续吸烟的女性的胎儿大小比不吸烟的女性小。持续吸烟者的胎儿尺寸减小遵循剂量依赖性模式(与非吸烟者相比,妊娠 40 周时平均 EFW [95% CI] 的差异为 -144 g [-182 至 -106],-215 g [- 248 到 -182] 和 -290 g [-334 到 -247] 分别用于轻度、中度和重度吸烟)。总体而言,FL 的胎儿体积减小最为明显。妊娠早期戒烟妇女的胎儿生长轨迹与非吸烟者相似,只是在妊娠 36-40 周左右,FL 较短,AC 较大。在 MR 分析中,基因决定的每天增加 1 支香烟与吸烟者从妊娠 20 周到出生的 EFW 较小相关(p = 0.01,40 周时平均 EFW 的差异 = -45 g [95% CI -81 到 -10]),并且从妊娠 32 周开始,非吸烟者的 EFW 更高(p = 0.03,40 周时平均 EFW 的差异 = 26 g [95% CI 5 至 47])。没有证据表明伴侣吸烟与胎儿生长有关。研究限制包括由于母亲自我报告吸烟导致的测量误差和 MR 分析的适度样本量导致无混淆的估计不太精确。遗传工具与非吸烟者胎儿生长的明显正相关表明遗传多效性可能掩盖了吸烟者更强的关联。结论 从妊娠中期早期开始观察到母亲吸烟与胎儿生长呈一致的线性剂量依赖性关联,而在妊娠早期戒烟的女性中没有发现主要的生长缺陷,除了妊娠晚期的 FL 较短。











































 京公网安备 11010802027423号
京公网安备 11010802027423号