当前位置:
X-MOL 学术
›
Modern Pathol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Metachronous intraductal papillary mucinous neoplasms disseminate via the pancreatic duct following resection.
Modern Pathology ( IF 7.1 ) Pub Date : 2019-11-13 , DOI: 10.1038/s41379-019-0405-7 Kazumasa Nagai 1, 2 , Yusuke Mizukami 3, 4 , Yuko Omori 5, 6 , Toshifumi Kin 1 , Kei Yane 1 , Kuniyuki Takahashi 1 , Yusuke Ono 3 , Ayumu Sugitani 3 , Hidenori Karasaki 3 , Toshiya Shinohara 5 , Toru Furukawa 6 , Tsuyoshi Hayashi 1 , Toshikatsu Okumura 4 , Hiroyuki Maguchi 1 , Akio Katanuma 1
Modern Pathology ( IF 7.1 ) Pub Date : 2019-11-13 , DOI: 10.1038/s41379-019-0405-7 Kazumasa Nagai 1, 2 , Yusuke Mizukami 3, 4 , Yuko Omori 5, 6 , Toshifumi Kin 1 , Kei Yane 1 , Kuniyuki Takahashi 1 , Yusuke Ono 3 , Ayumu Sugitani 3 , Hidenori Karasaki 3 , Toshiya Shinohara 5 , Toru Furukawa 6 , Tsuyoshi Hayashi 1 , Toshikatsu Okumura 4 , Hiroyuki Maguchi 1 , Akio Katanuma 1
Affiliation
|
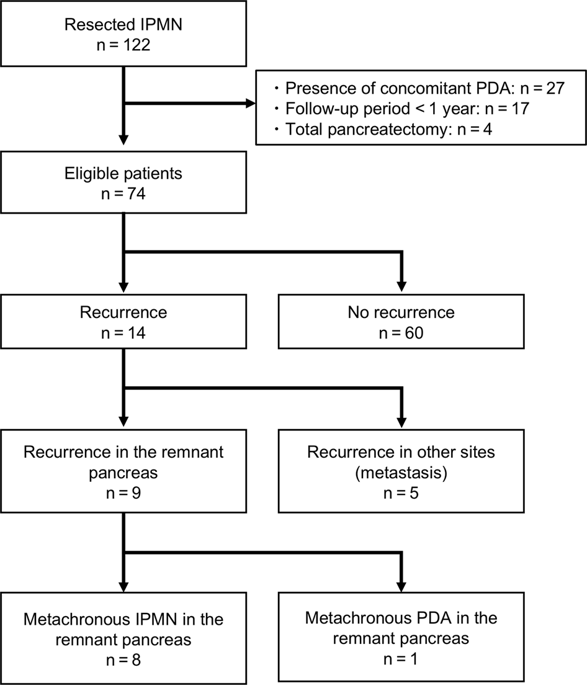
Metachronous development of intraductal papillary mucinous neoplasms in the remnant pancreas following resection is a significant clinical burden. Our aim was to characterize the clinicopathological and molecular features of the patients with metachronous tumor development to identify predictive factors and the possible route(s) of dissemination. Seventy-four patients who underwent resection of intraductal papillary mucinous neoplasms with no invasive compartment or associated carcinoma were retrospectively analyzed. In patients with metachronous tumor development, targeted sequencing of 18 genes associated with pancreatic tumorigenesis and immunohistochemical detection of four proteins (p53, SMAD4, p16, and β-catenin) were performed on both primary and metachronous tumors. The distributions of microscopic neoplastic lesions were examined at surgical margins and in apparently normal tissue apart from the primary tumor. During the median follow-up period of 52 months, 9 patients (12%) developed metachronous tumors in the remnant pancreas. Primary tumors located in the body/tail of the pancreas (odds ratio, 15; 95% confidence interval, 1.6-131) and of the pancreatobiliary type (odds ratio, 6.1; 95% confidence interval, 1.1-35.7) were identified as significant risk factors for subsequent metachronous tumor development. Eight of the nine patients shared molecular aberrations between their primary and metachronous tumors, suggesting migrations from the primary tumor to the pancreatic duct as the cause of metachronous tumor development. Our data suggest that these post-resection metachronous tumors develop by skip dissemination of the primary tumor, potentially via the pancreatic duct. The development of strategies to better predict and prevent this form of tumor progression is necessary.
中文翻译:

异时性导管内乳头状粘液性肿瘤在切除后通过胰管传播。
切除后残余胰腺中导管内乳头状粘液性肿瘤的异时性发展是一个重大的临床负担。我们的目的是描述异时性肿瘤发展患者的临床病理学和分子特征,以确定预测因素和可能的传播途径。回顾性分析了 74 例接受导管内乳头状粘液性肿瘤切除术且无浸润性隔室或相关癌的患者。在患有异时性肿瘤发展的患者中,对原发性和异时性肿瘤进行了 18 个与胰腺肿瘤发生相关的基因的靶向测序和四种蛋白质(p53、SMAD4、p16 和 β-连环蛋白)的免疫组织化学检测。在手术切缘和除原发肿瘤外的明显正常组织中检查微观肿瘤病变的分布。在 52 个月的中位随访期间,9 名患者 (12%) 在残余胰腺中发展为异时性肿瘤。位于胰腺体/尾的原发性肿瘤(比值比,15;95% 置信区间,1.6-131)和胰胆管类型(比值比,6.1;95% 置信区间,1.1-35.7)被确定为显着随后发生异时性肿瘤的危险因素。九名患者中有八名在原发性和异时性肿瘤之间存在分子畸变,这表明从原发性肿瘤向胰管的迁移是异时性肿瘤发展的原因。我们的数据表明,这些切除后的异时性肿瘤是通过原发肿瘤的跳跃传播而发展起来的,可能是通过胰管。有必要制定更好地预测和预防这种形式的肿瘤进展的策略。
更新日期:2019-11-13
中文翻译:

异时性导管内乳头状粘液性肿瘤在切除后通过胰管传播。
切除后残余胰腺中导管内乳头状粘液性肿瘤的异时性发展是一个重大的临床负担。我们的目的是描述异时性肿瘤发展患者的临床病理学和分子特征,以确定预测因素和可能的传播途径。回顾性分析了 74 例接受导管内乳头状粘液性肿瘤切除术且无浸润性隔室或相关癌的患者。在患有异时性肿瘤发展的患者中,对原发性和异时性肿瘤进行了 18 个与胰腺肿瘤发生相关的基因的靶向测序和四种蛋白质(p53、SMAD4、p16 和 β-连环蛋白)的免疫组织化学检测。在手术切缘和除原发肿瘤外的明显正常组织中检查微观肿瘤病变的分布。在 52 个月的中位随访期间,9 名患者 (12%) 在残余胰腺中发展为异时性肿瘤。位于胰腺体/尾的原发性肿瘤(比值比,15;95% 置信区间,1.6-131)和胰胆管类型(比值比,6.1;95% 置信区间,1.1-35.7)被确定为显着随后发生异时性肿瘤的危险因素。九名患者中有八名在原发性和异时性肿瘤之间存在分子畸变,这表明从原发性肿瘤向胰管的迁移是异时性肿瘤发展的原因。我们的数据表明,这些切除后的异时性肿瘤是通过原发肿瘤的跳跃传播而发展起来的,可能是通过胰管。有必要制定更好地预测和预防这种形式的肿瘤进展的策略。











































 京公网安备 11010802027423号
京公网安备 11010802027423号