Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of Transplant Center With Survival Benefit Among Adults Undergoing Heart Transplant in the United States
JAMA ( IF 63.1 ) Pub Date : 2019-11-12 , DOI: 10.1001/jama.2019.15686 William F Parker 1, 2, 3 , Allen S Anderson 4 , Robert D Gibbons 1, 3 , Edward R Garrity 1, 2 , Lainie F Ross 2, 5 , Elbert S Huang 1, 2 , Matthew M Churpek 1, 3
JAMA ( IF 63.1 ) Pub Date : 2019-11-12 , DOI: 10.1001/jama.2019.15686 William F Parker 1, 2, 3 , Allen S Anderson 4 , Robert D Gibbons 1, 3 , Edward R Garrity 1, 2 , Lainie F Ross 2, 5 , Elbert S Huang 1, 2 , Matthew M Churpek 1, 3
Affiliation
|
Importance
In the United States, the number of deceased donor hearts available for transplant is limited. As a proxy for medical urgency, the US heart allocation system ranks heart transplant candidates largely according to the supportive therapy prescribed by transplant centers. Objective
To determine if there is a significant association between transplant center and survival benefit in the US heart allocation system. Design, Setting, and Participants
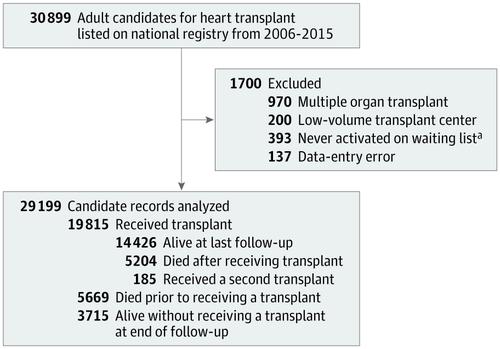
Observational study of 29 199 adult candidates for heart transplant listed on the national transplant registry from January 2006 through December 2015 with follow-up complete through August 2018. Exposures
Transplant center. Main Outcomes and Measures
The survival benefit associated with heart transplant as defined by the difference between survival after heart transplant and waiting list survival without transplant at 5 years. Each transplant center's mean survival benefit was estimated using a mixed-effects proportional hazards model with transplant as a time-dependent covariate, adjusted for year of transplant, donor quality, ischemic time, and candidate status. Results
Of 29 199 candidates (mean age, 52 years; 26% women) on the transplant waiting list at 113 centers, 19 815 (68%) underwent heart transplant. Among heart transplant recipients, 5389 (27%) died or underwent another transplant operation during the study period. Of the 9384 candidates who did not undergo heart transplant, 5669 (60%) died (2644 while on the waiting list and 3025 after being delisted). Estimated 5-year survival was 77% (interquartile range [IQR], 74% to 80%) among transplant recipients and 33% (IQR, 17% to 51%) among those who did not undergo heart transplant, which is a survival benefit of 44% (IQR, 27% to 59%). Survival benefit ranged from 30% to 55% across centers and 31 centers (27%) had significantly higher survival benefit than the mean and 30 centers (27%) had significantly lower survival benefit than the mean. Compared with low survival benefit centers, high survival benefit centers performed heart transplant for patients with lower estimated expected waiting list survival without transplant (29% at high survival benefit centers vs 39% at low survival benefit centers; survival difference, -10% [95% CI, -12% to -8.1%]), although the adjusted 5-year survival after transplant was not significantly different between high and low survival benefit centers (77.6% vs 77.1%, respectively; survival difference, 0.5% [95% CI, -1.3% to 2.3%]). Overall, for every 10% decrease in estimated transplant candidate waiting list survival at a given center, there was an increase of 6.2% (95% CI, 5.2% to 7.3%) in the 5-year survival benefit associated with heart transplant. Conclusions and Relevance
In this registry-based study of US heart transplant candidates, transplant center was associated with the survival benefit of transplant. Although the adjusted 5-year survival after transplant was not significantly different between high and low survival benefit centers, compared with centers with survival benefit significantly below the mean, centers with survival benefit significantly above the mean performed heart transplant for recipients who had significantly lower estimated expected 5-year waiting list survival without transplant.
中文翻译:

移植中心协会在美国接受心脏移植的成年人中具有生存益处
重要性 在美国,可用于移植的已故捐献心脏的数量是有限的。作为医疗紧急性的代表,美国心脏分配系统主要根据移植中心规定的支持疗法对心脏移植候选者进行排名。目的 确定美国心脏分配系统中移植中心与生存获益之间是否存在显着关联。设计、设置和参与者 对 2006 年 1 月至 2015 年 12 月在国家移植登记处列出的 29 199 名成人心脏移植候选者进行的观察性研究,随访完成至 2018 年 8 月。暴露移植中心。主要结果和措施 与心脏移植相关的生存获益定义为心脏移植后的生存与未进行移植的 5 年等待名单生存之间的差异。每个移植中心的平均生存获益是使用混合效应比例风险模型估计的,移植作为时间依赖的协变量,根据移植年份、供体质量、缺血时间和候选状态进行调整。结果 在 113 个中心的移植等待名单上的 29 199 名候选人(平均年龄,52 岁;26% 为女性)中,19 815 名(68%)接受了心脏移植。在心脏移植受者中,5389 人(27%)在研究期间死亡或接受了另一次移植手术。在未接受心脏移植的 9384 名候选人中,5669 人(60%)死亡(2644 人在等待名单上,3025 人在被除名后)。移植受者的估计 5 年生存率为 77%(四分位距 [IQR],74% 至 80%),未接受心脏移植者的估计 5 年生存率为 33%(IQR,17% 至 51%),这是一项生存获益44%(IQR,27% 至 59%)。各中心的生存获益范围为 30% 至 55%,31 个中心 (27%) 的生存获益显着高于平均值,30 个中心 (27%) 的生存获益显着低于平均值。与低生存获益中心相比,高生存获益中心对未经移植的预计预期等待名单生存率较低的患者进行心脏移植(高生存获益中心为 29%,低生存获益中心为 39%;生存差异,-10% [95] % CI,-12% 到 -8.1%]),尽管移植后调整后的 5 年生存率在高生存和低生存获益中心之间没有显着差异(分别为 77.6% 和 77.1%;生存差异,0.5% [95% CI,-1.3% 到 2.3%])。总体而言,在给定中心,预计移植候补名单存活率每降低 10%,与心脏移植相关的 5 年存活率就会增加 6.2%(95% CI,5.2% 至 7.3%)。结论和相关性 在这项针对美国心脏移植候选者的注册研究中,移植中心与移植的生存获益相关。尽管移植后调整后的 5 年生存率在高和低生存获益中心之间没有显着差异,但与生存获益显着低于平均值的中心相比,
更新日期:2019-11-12
中文翻译:

移植中心协会在美国接受心脏移植的成年人中具有生存益处
重要性 在美国,可用于移植的已故捐献心脏的数量是有限的。作为医疗紧急性的代表,美国心脏分配系统主要根据移植中心规定的支持疗法对心脏移植候选者进行排名。目的 确定美国心脏分配系统中移植中心与生存获益之间是否存在显着关联。设计、设置和参与者 对 2006 年 1 月至 2015 年 12 月在国家移植登记处列出的 29 199 名成人心脏移植候选者进行的观察性研究,随访完成至 2018 年 8 月。暴露移植中心。主要结果和措施 与心脏移植相关的生存获益定义为心脏移植后的生存与未进行移植的 5 年等待名单生存之间的差异。每个移植中心的平均生存获益是使用混合效应比例风险模型估计的,移植作为时间依赖的协变量,根据移植年份、供体质量、缺血时间和候选状态进行调整。结果 在 113 个中心的移植等待名单上的 29 199 名候选人(平均年龄,52 岁;26% 为女性)中,19 815 名(68%)接受了心脏移植。在心脏移植受者中,5389 人(27%)在研究期间死亡或接受了另一次移植手术。在未接受心脏移植的 9384 名候选人中,5669 人(60%)死亡(2644 人在等待名单上,3025 人在被除名后)。移植受者的估计 5 年生存率为 77%(四分位距 [IQR],74% 至 80%),未接受心脏移植者的估计 5 年生存率为 33%(IQR,17% 至 51%),这是一项生存获益44%(IQR,27% 至 59%)。各中心的生存获益范围为 30% 至 55%,31 个中心 (27%) 的生存获益显着高于平均值,30 个中心 (27%) 的生存获益显着低于平均值。与低生存获益中心相比,高生存获益中心对未经移植的预计预期等待名单生存率较低的患者进行心脏移植(高生存获益中心为 29%,低生存获益中心为 39%;生存差异,-10% [95] % CI,-12% 到 -8.1%]),尽管移植后调整后的 5 年生存率在高生存和低生存获益中心之间没有显着差异(分别为 77.6% 和 77.1%;生存差异,0.5% [95% CI,-1.3% 到 2.3%])。总体而言,在给定中心,预计移植候补名单存活率每降低 10%,与心脏移植相关的 5 年存活率就会增加 6.2%(95% CI,5.2% 至 7.3%)。结论和相关性 在这项针对美国心脏移植候选者的注册研究中,移植中心与移植的生存获益相关。尽管移植后调整后的 5 年生存率在高和低生存获益中心之间没有显着差异,但与生存获益显着低于平均值的中心相比,










































 京公网安备 11010802027423号
京公网安备 11010802027423号