当前位置:
X-MOL 学术
›
Adv. Healthcare Mater.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Vascular Pedicle and Microchannels: Simple Methods Toward Effective In Vivo Vascularization of 3D Scaffolds.
Advanced Healthcare Materials ( IF 10.0 ) Pub Date : 2019-11-12 , DOI: 10.1002/adhm.201901106 Jelena Rnjak-Kovacina 1, 2 , Yi-Wen Gerrand 3 , Lindsay S Wray 1 , Beryl Tan 3 , Habib Joukhdar 2 , David L Kaplan 1 , Wayne A Morrison 3, 4, 5 , Geraldine M Mitchell 3, 4, 5
Advanced Healthcare Materials ( IF 10.0 ) Pub Date : 2019-11-12 , DOI: 10.1002/adhm.201901106 Jelena Rnjak-Kovacina 1, 2 , Yi-Wen Gerrand 3 , Lindsay S Wray 1 , Beryl Tan 3 , Habib Joukhdar 2 , David L Kaplan 1 , Wayne A Morrison 3, 4, 5 , Geraldine M Mitchell 3, 4, 5
Affiliation
|
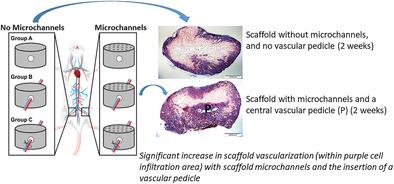
Poor vascularization remains a key limiting factor in translating advances in tissue engineering to clinical applications. Vascular pedicles (large arteries and veins) isolated in plastic chambers are known to sprout an extensive capillary network. This study examined the effect vascular pedicles and scaffold architecture have on vascularization and tissue integration of implanted silk scaffolds. Porous silk scaffolds with or without microchannels are manufactured to support implantation of a central vascular pedicle, without a chamber, implanted in the groin of Sprague Dawley rats, and assessed morphologically and morphometrically at 2 and 6 weeks. At both time points, blood vessels, connective tissue, and an inflammatory response infiltrate all scaffold pores externally, and centrally when a vascular pedicle is implanted. At week 2, vascular pedicles significantly increase the degree of scaffold tissue infiltration, and both the pedicle and the scaffold microchannels significantly increase vascular volume and vascular density. Interestingly, microchannels contribute to increased scaffold vascularity without affecting overall tissue infiltration, suggesting a direct effect of biomaterial architecture on vascularization. The inclusion of pedicles and microchannels are simple and effective proangiogenic techniques for engineering thick tissue constructs as both increase the speed of construct vascularization in the early weeks post in vivo implantation.
中文翻译:

血管蒂和微通道:简便有效的3D支架体内血管化方法。
血管生成不良仍然是将组织工程学进展转化为临床应用的关键限制因素。隔离在塑料腔中的血管蒂(大动脉和静脉)会萌生出广泛的毛细管网络。这项研究检查了血管蒂和支架结构对植入的丝支架的血管化和组织整合的影响。制造具有或不具有微通道的多孔丝支架,以支持不带腔室的中央血管蒂的植入,植入Sprague Dawley大鼠的腹股沟,并在2和6周时进行形态学和形态学评估。在两个时间点,当植入血管蒂时,血管,结缔组织和炎症反应都会从外部和中央渗透到所有支架孔中。在第二周 血管蒂显着增加了支架组织的浸润程度,并且蒂和支架微通道都显着增加了血管体积和血管密度。有趣的是,微通道有助于增加支架的血管,而不会影响整个组织的浸润,表明生物材料结构对血管形成有直接影响。包含蒂和微通道是用于工程化厚组织构造物的简单有效的促血管生成技术,因为两者均增加了在体内植入后早期构造物血管化的速度。微通道有助于增加支架的血管,而不会影响整个组织的浸润,表明生物材料结构对血管化有直接影响。包含蒂和微通道是用于工程化厚组织构造物的简单有效的促血管生成技术,因为两者均增加了在体内植入后早期构造物血管化的速度。微通道有助于增加支架的血管,而不会影响整个组织的浸润,表明生物材料结构对血管化具有直接作用。包含蒂和微通道是用于工程化厚组织构造物的简单有效的促血管生成技术,因为两者均增加了在体内植入后早期构造物血管化的速度。
更新日期:2019-12-19
中文翻译:

血管蒂和微通道:简便有效的3D支架体内血管化方法。
血管生成不良仍然是将组织工程学进展转化为临床应用的关键限制因素。隔离在塑料腔中的血管蒂(大动脉和静脉)会萌生出广泛的毛细管网络。这项研究检查了血管蒂和支架结构对植入的丝支架的血管化和组织整合的影响。制造具有或不具有微通道的多孔丝支架,以支持不带腔室的中央血管蒂的植入,植入Sprague Dawley大鼠的腹股沟,并在2和6周时进行形态学和形态学评估。在两个时间点,当植入血管蒂时,血管,结缔组织和炎症反应都会从外部和中央渗透到所有支架孔中。在第二周 血管蒂显着增加了支架组织的浸润程度,并且蒂和支架微通道都显着增加了血管体积和血管密度。有趣的是,微通道有助于增加支架的血管,而不会影响整个组织的浸润,表明生物材料结构对血管形成有直接影响。包含蒂和微通道是用于工程化厚组织构造物的简单有效的促血管生成技术,因为两者均增加了在体内植入后早期构造物血管化的速度。微通道有助于增加支架的血管,而不会影响整个组织的浸润,表明生物材料结构对血管化有直接影响。包含蒂和微通道是用于工程化厚组织构造物的简单有效的促血管生成技术,因为两者均增加了在体内植入后早期构造物血管化的速度。微通道有助于增加支架的血管,而不会影响整个组织的浸润,表明生物材料结构对血管化具有直接作用。包含蒂和微通道是用于工程化厚组织构造物的简单有效的促血管生成技术,因为两者均增加了在体内植入后早期构造物血管化的速度。











































 京公网安备 11010802027423号
京公网安备 11010802027423号