当前位置:
X-MOL 学术
›
Kidney Int.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Blood pressure modifies outcomes in patients with stage 3 to 5 chronic kidney disease.
Kidney International ( IF 19.6 ) Pub Date : 2019-11-07 , DOI: 10.1016/j.kint.2019.10.021 Heng-Pin Chiang , Yi-Wen Chiu , Jia-Jung Lee , Chi-Chih Hung , Shang-Jyh Hwang , Hung-Chun Chen
Kidney International ( IF 19.6 ) Pub Date : 2019-11-07 , DOI: 10.1016/j.kint.2019.10.021 Heng-Pin Chiang , Yi-Wen Chiu , Jia-Jung Lee , Chi-Chih Hung , Shang-Jyh Hwang , Hung-Chun Chen
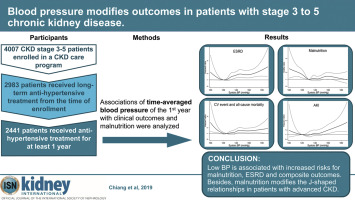
|
Observational studies have demonstrated that low blood pressure is related to poor clinical outcomes in patients with chronic kidney disease (CKD). Subgroup analyses from the SPRINT trial showed that targeting systolic blood pressure under 120 mmHg is less beneficial for patients with CKD. Although malnutrition and inflammation are common in patients with advanced CKD, such patients are usually excluded from clinical trials. Therefore, we hypothesized that malnutrition-inflammation-cachexia syndrome could explain this J-shaped relationship. To test this, we studied 2441 patients with CKD stages 3-5 who received anti-hypertensive treatment for at least one year. Averaged blood pressures of the first year were used in the analyses. Fine-Gray competing risks regression showed a J-shaped relationship between continuous systolic blood pressure and end-stage kidney disease (ESKD) with a nadir risk at a systolic blood pressure of 120 mmHg. Adjusted sub-distribution hazard ratios of categorical systolic blood pressure 100-109 and 110-119 mmHg were 2.17 (95% confidence interval: 1.21-3.89) and 1.37 (0.94-1.99) for ESKD, respectively, compared with systolic blood pressures of 120-129 mmHg. Cox regression also showed J-shaped relationships between continuous systolic or diastolic blood pressures, and the composite outcomes of cardiovascular events and all-cause mortality. Logistic regression demonstrated the odds ratios of blood pressure components for Malnutrition-Inflammation Scores over 4 were J-shaped. Sub-distribution hazard ratios of systolic blood pressure 100-119 mmHg for ESKD was higher in those with a Malnutrition-Inflammation Score over 4, compared to 0.93 (0.53-1.63) in those with a score of 4 or under with significant interaction. Thus, malnutrition-inflammation-cachexia syndrome is associated with low blood pressure and modifies the J-shaped relationship in patients with advanced CKD.
中文翻译:

血压会改变3至5期慢性肾脏病患者的结局。
观察性研究表明,低血压与慢性肾脏病(CKD)患者的临床预后不良有关。SPRINT试验的亚组分析表明,将收缩压控制在120 mmHg以下对CKD患者的益处较小。尽管营养不良和炎症在晚期CKD患者中很常见,但此类患者通常被排除在临床试验之外。因此,我们假设营养不良-炎症-恶病质综合征可以解释这种J型关系。为了测试这一点,我们研究了2441例3-5 CKD的患者,他们接受了至少一年的降压治疗。分析中使用了第一年的平均血压。精细灰色竞争风险回归表明,连续收缩压与终末期肾脏疾病(ESKD)之间呈J形关系,收缩压为120 mmHg时为最低风险。对于ESKD,分类收缩压为100-109和110-119 mmHg的子分布危险比分别为2.17(95%置信区间:1.21-3.89)和1.37(0.94-1.99),而收缩压为120 -129毫米汞柱。Cox回归还显示连续收缩压或舒张压与心血管事件和全因死亡率的复合结果之间呈J形关系。Logistic回归显示,营养不良-炎症评分超过4的血压成分的优势比为J形。营养不良评分超过4的人群的ESKD收缩压的子分布危险比为100-119 mmHg,高于4或低于4且相互作用明显的人群的0.93(0.53-1.63)。因此,营养不良-炎症-恶病质综合征与低血压有关,并改变了晚期CKD患者的J形关系。
更新日期:2019-11-08
中文翻译:

血压会改变3至5期慢性肾脏病患者的结局。
观察性研究表明,低血压与慢性肾脏病(CKD)患者的临床预后不良有关。SPRINT试验的亚组分析表明,将收缩压控制在120 mmHg以下对CKD患者的益处较小。尽管营养不良和炎症在晚期CKD患者中很常见,但此类患者通常被排除在临床试验之外。因此,我们假设营养不良-炎症-恶病质综合征可以解释这种J型关系。为了测试这一点,我们研究了2441例3-5 CKD的患者,他们接受了至少一年的降压治疗。分析中使用了第一年的平均血压。精细灰色竞争风险回归表明,连续收缩压与终末期肾脏疾病(ESKD)之间呈J形关系,收缩压为120 mmHg时为最低风险。对于ESKD,分类收缩压为100-109和110-119 mmHg的子分布危险比分别为2.17(95%置信区间:1.21-3.89)和1.37(0.94-1.99),而收缩压为120 -129毫米汞柱。Cox回归还显示连续收缩压或舒张压与心血管事件和全因死亡率的复合结果之间呈J形关系。Logistic回归显示,营养不良-炎症评分超过4的血压成分的优势比为J形。营养不良评分超过4的人群的ESKD收缩压的子分布危险比为100-119 mmHg,高于4或低于4且相互作用明显的人群的0.93(0.53-1.63)。因此,营养不良-炎症-恶病质综合征与低血压有关,并改变了晚期CKD患者的J形关系。



























 京公网安备 11010802027423号
京公网安备 11010802027423号