当前位置:
X-MOL 学术
›
JAMA Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Mind-Body Therapies for Opioid-Treated Pain
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamainternmed.2019.4917 Eric L Garland 1, 2 , Carrie E Brintz 3 , Adam W Hanley 1, 2 , Eric J Roseen 4, 5 , Rachel M Atchley 6 , Susan A Gaylord 3 , Keturah R Faurot 3 , Joanne Yaffe 2 , Michelle Fiander 7 , Francis J Keefe 8, 9, 10
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamainternmed.2019.4917 Eric L Garland 1, 2 , Carrie E Brintz 3 , Adam W Hanley 1, 2 , Eric J Roseen 4, 5 , Rachel M Atchley 6 , Susan A Gaylord 3 , Keturah R Faurot 3 , Joanne Yaffe 2 , Michelle Fiander 7 , Francis J Keefe 8, 9, 10
Affiliation
|
Importance
Mind-body therapies (MBTs) are emerging as potential tools for addressing the opioid crisis. Knowing whether mind-body therapies may benefit patients treated with opioids for acute, procedural, and chronic pain conditions may be useful for prescribers, payers, policy makers, and patients. Objective
To evaluate the association of MBTs with pain and opioid dose reduction in a diverse adult population with clinical pain. Data Sources
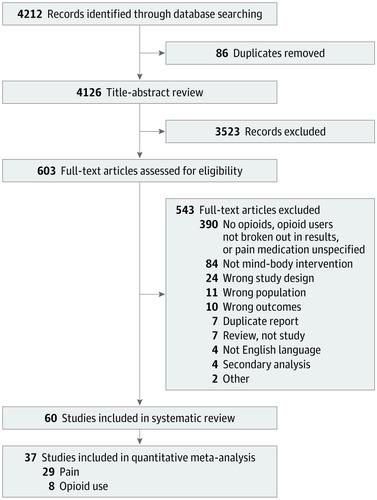
For this systematic review and meta-analysis, the MEDLINE, Embase, Emcare, CINAHL, PsycINFO, and Cochrane Library databases were searched for English-language randomized clinical trials and systematic reviews from date of inception to March 2018. Search logic included (pain OR analgesia OR opioids) AND mind-body therapies. The gray literature, ClinicalTrials.gov, and relevant bibliographies were also searched. Study Selection
Randomized clinical trials that evaluated the use of MBTs for symptom management in adults also prescribed opioids for clinical pain. Data Extraction and Synthesis
Independent reviewers screened citations, extracted data, and assessed risk of bias. Meta-analyses were conducted using standardized mean differences in pain and opioid dose to obtain aggregate estimates of effect size with 95% CIs. Main Outcomes and Measures
The primary outcome was pain intensity. The secondary outcomes were opioid dose, opioid misuse, opioid craving, disability, or function. Results
Of 4212 citations reviewed, 60 reports with 6404 participants were included in the meta-analysis. Overall, MBTs were associated with pain reduction (Cohen d = -0.51; 95% CI, -0.76 to -0.26) and reduced opioid dose (Cohen d = -0.26; 95% CI, -0.44 to -0.08). Studies tested meditation (n = 5), hypnosis (n = 25), relaxation (n = 14), guided imagery (n = 7), therapeutic suggestion (n = 6), and cognitive behavioral therapy (n = 7) interventions. Moderate to large effect size improvements in pain outcomes were found for meditation (Cohen d = -0.70), hypnosis (Cohen d = -0.54), suggestion (Cohen d = -0.68), and cognitive behavioral therapy (Cohen d = -0.43) but not for other MBTs. Although most meditation (n = 4 [80%]), cognitive-behavioral therapy (n = 4 [57%]), and hypnosis (n = 12 [63%]) studies found improved opioid-related outcomes, fewer studies of suggestion, guided imagery, and relaxation reported such improvements. Most MBT studies used active or placebo controls and were judged to be at low risk of bias. Conclusions and Relevance
The findings suggest that MBTs are associated with moderate improvements in pain and small reductions in opioid dose and may be associated with therapeutic benefits for opioid-related problems, such as opioid craving and misuse. Future studies should carefully quantify opioid dosing variables to determine the association of mind-body therapies with opioid-related outcomes.
中文翻译:

阿片类药物治疗疼痛的身心疗法
重要性 身心疗法 (MBT) 正在成为解决阿片类药物危机的潜在工具。了解身心疗法是否可以使接受阿片类药物治疗急性、手术性和慢性疼痛的患者受益,可能对处方者、付款者、政策制定者和患者有用。目的 评估不同成人临床疼痛人群中 MBT 与疼痛和阿片类药物剂量减少的关系。数据源 在本次系统评价和荟萃分析中,检索了 MEDLINE、Embase、Emcare、CINAHL、PsycINFO 和 Cochrane 图书馆数据库,以查找从开始之日起至 2018 年 3 月的英语随机临床试验和系统评价。搜索逻辑包括(疼痛或镇痛或阿片类药物)和身心疗法。还检索了灰色文献、ClinicalTrials.gov 和相关参考书目。研究选择 评估使用 MBT 治疗成人症状的随机临床试验也开出阿片类药物用于治疗临床疼痛。数据提取和综合独立审稿人筛选引文、提取数据并评估偏倚风险。使用疼痛和阿片类药物剂量的标准化平均差异进行荟萃分析,以获得效应大小的总体估计(95% CI)。主要结果和措施 主要结果是疼痛强度。次要结局是阿片类药物剂量、阿片类药物滥用、阿片类药物渴望、残疾或功能。结果 在审查的 4212 条引用中,60 份报告、6404 名参与者被纳入荟萃分析。总体而言,MBT 与减轻疼痛(Cohen d = -0.51;95% CI,-0.76 至 -0.26)和减少阿片类药物剂量(Cohen d = -0.26;95% CI,-0.44 至 -0.08)相关。 研究测试了冥想(n = 5)、催眠(n = 25)、放松(n = 14)、引导意象(n = 7)、治疗建议(n = 6)和认知行为疗法(n = 7)干预措施。冥想(科恩 d = -0.70)、催眠(科恩 d = -0.54)、建议(科恩 d = -0.68)和认知行为疗法(科恩 d = -0.43)对疼痛结果有中等到大的效果改善但不适用于其他主战坦克。尽管大多数冥想(n = 4 [80%])、认知行为疗法(n = 4 [57%])和催眠(n = 12 [63%])研究发现阿片类药物相关的结果有所改善,但建议研究较少、引导意象和放松报告了此类改进。大多数 MBT 研究使用活性或安慰剂对照,并被认为偏倚风险较低。结论和相关性 研究结果表明,MBT 与疼痛的适度改善和阿片类药物剂量的小幅减少有关,并且可能与阿片类药物相关问题(例如阿片类药物渴望和滥用)的治疗益处相关。未来的研究应仔细量化阿片类药物剂量变量,以确定身心疗法与阿片类药物相关结果的关联。
更新日期:2020-01-01
中文翻译:

阿片类药物治疗疼痛的身心疗法
重要性 身心疗法 (MBT) 正在成为解决阿片类药物危机的潜在工具。了解身心疗法是否可以使接受阿片类药物治疗急性、手术性和慢性疼痛的患者受益,可能对处方者、付款者、政策制定者和患者有用。目的 评估不同成人临床疼痛人群中 MBT 与疼痛和阿片类药物剂量减少的关系。数据源 在本次系统评价和荟萃分析中,检索了 MEDLINE、Embase、Emcare、CINAHL、PsycINFO 和 Cochrane 图书馆数据库,以查找从开始之日起至 2018 年 3 月的英语随机临床试验和系统评价。搜索逻辑包括(疼痛或镇痛或阿片类药物)和身心疗法。还检索了灰色文献、ClinicalTrials.gov 和相关参考书目。研究选择 评估使用 MBT 治疗成人症状的随机临床试验也开出阿片类药物用于治疗临床疼痛。数据提取和综合独立审稿人筛选引文、提取数据并评估偏倚风险。使用疼痛和阿片类药物剂量的标准化平均差异进行荟萃分析,以获得效应大小的总体估计(95% CI)。主要结果和措施 主要结果是疼痛强度。次要结局是阿片类药物剂量、阿片类药物滥用、阿片类药物渴望、残疾或功能。结果 在审查的 4212 条引用中,60 份报告、6404 名参与者被纳入荟萃分析。总体而言,MBT 与减轻疼痛(Cohen d = -0.51;95% CI,-0.76 至 -0.26)和减少阿片类药物剂量(Cohen d = -0.26;95% CI,-0.44 至 -0.08)相关。 研究测试了冥想(n = 5)、催眠(n = 25)、放松(n = 14)、引导意象(n = 7)、治疗建议(n = 6)和认知行为疗法(n = 7)干预措施。冥想(科恩 d = -0.70)、催眠(科恩 d = -0.54)、建议(科恩 d = -0.68)和认知行为疗法(科恩 d = -0.43)对疼痛结果有中等到大的效果改善但不适用于其他主战坦克。尽管大多数冥想(n = 4 [80%])、认知行为疗法(n = 4 [57%])和催眠(n = 12 [63%])研究发现阿片类药物相关的结果有所改善,但建议研究较少、引导意象和放松报告了此类改进。大多数 MBT 研究使用活性或安慰剂对照,并被认为偏倚风险较低。结论和相关性 研究结果表明,MBT 与疼痛的适度改善和阿片类药物剂量的小幅减少有关,并且可能与阿片类药物相关问题(例如阿片类药物渴望和滥用)的治疗益处相关。未来的研究应仔细量化阿片类药物剂量变量,以确定身心疗法与阿片类药物相关结果的关联。











































 京公网安备 11010802027423号
京公网安备 11010802027423号