当前位置:
X-MOL 学术
›
Kidney Int.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
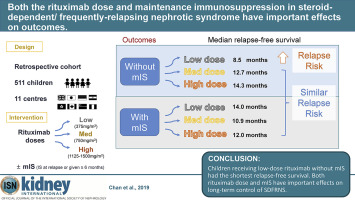
Both the rituximab dose and maintenance immunosuppression in steroid-dependent/frequently-relapsing nephrotic syndrome have important effects on outcomes.
Kidney International ( IF 14.8 ) Pub Date : 2019-10-31 , DOI: 10.1016/j.kint.2019.09.033 Eugene Yu-Hin Chan 1 , Hazel Webb 2 , Ellen Yu 3 , Gian Marco Ghiggeri 4 , Markus J Kemper 5 , Alison Lap-Tak Ma 6 , Tomohiko Yamamura 7 , Aditi Sinha 8 , Arvind Bagga 8 , Julien Hogan 9 , Claire Dossier 9 , Marina Vivarelli 10 , Isaac Desheng Liu 11 , Koichi Kamei 12 , Kenji Ishikura 13 , Priya Saini 14 , Kjell Tullus 2
Kidney International ( IF 14.8 ) Pub Date : 2019-10-31 , DOI: 10.1016/j.kint.2019.09.033 Eugene Yu-Hin Chan 1 , Hazel Webb 2 , Ellen Yu 3 , Gian Marco Ghiggeri 4 , Markus J Kemper 5 , Alison Lap-Tak Ma 6 , Tomohiko Yamamura 7 , Aditi Sinha 8 , Arvind Bagga 8 , Julien Hogan 9 , Claire Dossier 9 , Marina Vivarelli 10 , Isaac Desheng Liu 11 , Koichi Kamei 12 , Kenji Ishikura 13 , Priya Saini 14 , Kjell Tullus 2
Affiliation
|
Rituximab is an effective treatment for steroid-dependent/ frequently-relapsing nephrotic syndrome (SDFRNS) in children. However, the optimal rituximab regimen remains unknown. To help determine this we conducted an international, multicenter retrospective study at 11 tertiary pediatric nephrology centers in Asia, Europe and North America of children 1-18 years of age with complicated SDFRNS receiving rituximab between 2005-2016 for 18 or more months follow-up. The effect of rituximab prescribed at three dosing levels: low (375mg/m2), medium (750mg/m2) and high (1125-1500mg/m2), with or without maintenance immunosuppression (defined as concurrent use of corticosteroids, mycophenolate motile or calcineurin inhibition at first relapse or for at least six months following the rituximab treatment) was examined. Among the 511 children (median age 11.5 year, 67% boys), 191, 208 and 112 received low, medium and high dose rituximab, respectively. Within this total cohort of 511 children, 283 (55%) received maintenance immunosuppression. Renal biopsies were performed in 317 children indicating the predominant histology was minimal change disease (74%). Without maintenance immunosuppression, low-dose rituximab had a shorter relapse-free period and a higher relapse risk (8.5 months) than medium (12.7 months; adjusted hazard ratio, 0.62) and high dose (14.3 months; adjusted hazard ratio, 0.50; all significant). With maintenance immunosuppression, the relapse-free survival in low-dose rituximab (14 months) was similar to medium (10.9 months; adjusted hazard ratio, 1.23) and high dose (12.0 months; adjusted hazard ratio, 0.92; all non-significant). Most adverse events were mild. Thus, children receiving low-dose rituximab without maintenance immunosuppression had the shortest relapse-free survival. Hence, both rituximab dose and maintenance immunosuppression have important effects on the treatment outcomes.
中文翻译:

激素依赖/频发性肾病综合征的利妥昔单抗剂量和维持性免疫抑制均对预后产生重要影响。
利妥昔单抗是治疗儿童类固醇依赖/经常复发的肾病综合征(SDFRNS)的有效方法。但是,最佳的利妥昔单抗治疗方案仍然未知。为了帮助确定这一点,我们在亚洲,欧洲和北美洲的11个三级儿童肾脏病中心进行了一项国际,多中心回顾性研究,研究对象为2005年至2016年间接受SD的NSFRNS患者,年龄在1-18岁之间,并接受了利妥昔单抗治疗18个月或更长时间。三种剂量的利妥昔单抗的疗效:低(375mg / m2),中(750mg / m2)和高(1125-1500mg / m2),有或没有维持免疫抑制作用(定义为同时使用皮质类固醇,霉酚酸酯或钙调神经磷酸酶)检查了首次复发时或利妥昔单抗治疗后至少六个月的抑制作用。在511名儿童(中位年龄为11岁)中 5岁,67%的男孩,191、208和112分别接受了低剂量,中剂量和高剂量利妥昔单抗治疗。在这511名儿童中,有283名(55%)接受了维持性免疫抑制。对317名儿童进行了肾脏活检,表明主要的组织学是最小变化疾病(74%)。没有维持性免疫抑制,低剂量利妥昔单抗的无复发期较短,复发风险(8.5个月)高于中度(12.7个月;危险比调整为0.62)和高剂量(14.3个月;危险比调整为0.50;全部)重大)。在维持免疫抑制的情况下,低剂量利妥昔单抗(14个月)的无复发存活率与中等(10.9个月;危险比调整为1.23)和高剂量(12.0个月;危险比调整为0.92;所有无显着性)相似。 。大多数不良事件是轻度的。因此,接受低剂量利妥昔单抗但未维持免疫抑制的儿童,其无复发生存期最短。因此,利妥昔单抗剂量和维持免疫抑制均对治疗结果具有重要影响。
更新日期:2019-11-01
中文翻译:

激素依赖/频发性肾病综合征的利妥昔单抗剂量和维持性免疫抑制均对预后产生重要影响。
利妥昔单抗是治疗儿童类固醇依赖/经常复发的肾病综合征(SDFRNS)的有效方法。但是,最佳的利妥昔单抗治疗方案仍然未知。为了帮助确定这一点,我们在亚洲,欧洲和北美洲的11个三级儿童肾脏病中心进行了一项国际,多中心回顾性研究,研究对象为2005年至2016年间接受SD的NSFRNS患者,年龄在1-18岁之间,并接受了利妥昔单抗治疗18个月或更长时间。三种剂量的利妥昔单抗的疗效:低(375mg / m2),中(750mg / m2)和高(1125-1500mg / m2),有或没有维持免疫抑制作用(定义为同时使用皮质类固醇,霉酚酸酯或钙调神经磷酸酶)检查了首次复发时或利妥昔单抗治疗后至少六个月的抑制作用。在511名儿童(中位年龄为11岁)中 5岁,67%的男孩,191、208和112分别接受了低剂量,中剂量和高剂量利妥昔单抗治疗。在这511名儿童中,有283名(55%)接受了维持性免疫抑制。对317名儿童进行了肾脏活检,表明主要的组织学是最小变化疾病(74%)。没有维持性免疫抑制,低剂量利妥昔单抗的无复发期较短,复发风险(8.5个月)高于中度(12.7个月;危险比调整为0.62)和高剂量(14.3个月;危险比调整为0.50;全部)重大)。在维持免疫抑制的情况下,低剂量利妥昔单抗(14个月)的无复发存活率与中等(10.9个月;危险比调整为1.23)和高剂量(12.0个月;危险比调整为0.92;所有无显着性)相似。 。大多数不良事件是轻度的。因此,接受低剂量利妥昔单抗但未维持免疫抑制的儿童,其无复发生存期最短。因此,利妥昔单抗剂量和维持免疫抑制均对治疗结果具有重要影响。











































 京公网安备 11010802027423号
京公网安备 11010802027423号