当前位置:
X-MOL 学术
›
JAMA Surg.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association Between Bariatric Surgery and Long-term Health Care Expenditures Among Veterans With Severe Obesity.
JAMA Surgery ( IF 15.7 ) Pub Date : 2019-12-18 , DOI: 10.1001/jamasurg.2019.3732 Valerie A Smith 1, 2, 3 , David E Arterburn 4, 5 , Theodore S Z Berkowitz 1 , Maren K Olsen 1, 6 , Edward H Livingston 7, 8, 9 , William S Yancy 1, 3 , Hollis J Weidenbacher 1 , Matthew L Maciejewski 1, 2, 3
JAMA Surgery ( IF 15.7 ) Pub Date : 2019-12-18 , DOI: 10.1001/jamasurg.2019.3732 Valerie A Smith 1, 2, 3 , David E Arterburn 4, 5 , Theodore S Z Berkowitz 1 , Maren K Olsen 1, 6 , Edward H Livingston 7, 8, 9 , William S Yancy 1, 3 , Hollis J Weidenbacher 1 , Matthew L Maciejewski 1, 2, 3
Affiliation
|
Importance
Bariatric surgery has been associated with improvements in health in patients with severe obesity; however, it is unclear whether these health benefits translate into lower health care expenditures.
Objective
To examine 10-year health care expenditures in a large, multisite retrospective cohort study of veterans with severe obesity who did and did not undergo bariatric surgery.
Design, Setting, and Participants
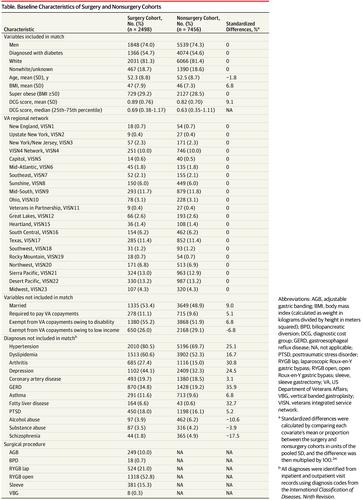
A total of 9954 veterans with severe obesity between January 1, 2000, and September 30, 2011, were identified from veterans affairs (VA) electronic health records. Of those, 2498 veterans who underwent bariatric surgery were allocated to the surgery cohort. Sequential stratification was used to match each patient in the surgery cohort with up to 3 patients who had not undergone bariatric surgery but were of the same sex, race/ethnicity, diabetes status, and VA regional network and were closest in age, body mass index (calculated as weight in kilograms divided by height in meters squared), and comorbidities. A total of 7456 patients were identified and allocated to the nonsurgery (control) cohort. The VA health care expenditures among the surgery and nonsurgery cohorts were estimated using regression models. Data were analyzed from July to August 2018 and in April 2019.
Interventions
The bariatric surgical procedures (n = 2498) included in this study were Roux-en-Y gastric bypass (1842 [73.7%]), sleeve gastrectomy (381 [15.3%]), adjustable gastric banding (249 [10.0%]), and other procedures (26 [1.0%]).
Main Outcomes and Measures
The study measured total, outpatient, inpatient, and outpatient pharmacy expenditures from 3 years before surgery to 10 years after surgery, excluding expenditures associated with the initial bariatric surgical procedure.
Results
Among 9954 veterans with severe obesity, 7387 (74.2%) were men; the mean (SD) age was 52.3 (8.8) years for the surgery cohort and 52.5 (8.7) years for the nonsurgery cohort. Mean total expenditures for the surgery cohort were $5093 (95% CI, $4811-$5391) at 7 to 12 months before surgery, which increased to $7448 (95% CI, $6989-$7936) at 6 months after surgery. Postsurgical expenditures decreased to $6692 (95% CI, $6197-$7226) at 5 years after surgery, followed by a gradual increase to $8495 (95% CI, $7609-$9484) at 10 years after surgery. Total expenditures were higher in the surgery cohort than in the nonsurgery cohort during the 3 years before surgery and in the first 2 years after surgery. The expenditures of the 2 cohorts converged 5 to 10 years after surgery. Outpatient pharmacy expenditures were significantly lower among the surgery cohort in all years of follow-up ($509 lower at 3 years before surgery and $461 lower at 7 to 12 months before surgery), but these cost reductions were offset by higher inpatient and outpatient (nonpharmacy) expenditures.
Conclusions and Relevance
In this cohort study of 9954 predominantly older male veterans with severe obesity, total health care expenditures increased immediately after patients underwent bariatric surgery but converged with those of patients who had not undergone surgery at 10 years after surgery. This finding suggests that the value of bariatric surgery lies primarily in its associations with improvements in health and not in its potential to decrease health care costs.
中文翻译:

肥胖症退伍军人中的减肥手术与长期医疗保健支出之间的关联。
重要性减肥手术已与重度肥胖患者的健康状况改善相关。但是,尚不清楚这些健康益处是否会转化为较低的医疗保健支出。目的在一项大型,多地点回顾性队列研究中,对接受过肥胖手术和不接受肥胖手术的退伍军人进行一项为期十年的大型回顾性队列研究,以研究其十年的医疗保健支出。设计,设置和参与者从退伍军人事务(VA)电子健康记录中识别出了2000年1月1日至2011年9月30日期间共有9954名严重肥胖的退伍军人。在这些人中,有2498名接受了减肥手术的退伍军人被分配到该手术队列中。依序进行分层,以使手术队列中的每位患者与最多3例未进行过减肥手术但性别相同的患者相匹配,种族/族裔,糖尿病状况和VA区域网络,并且年龄,体重指数(以体重(公斤)除以身高(米为平方)计算)和合并症最接近。总共确定了7456例患者,并将其分配到非手术(对照)队列中。使用回归模型估算了手术和非手术人群中的VA保健支出。分析了2018年7月至2018年8月以及2019年4月的数据。干预措施这项研究中包括的减肥手术方法(n = 2498)为Roux-en-Y胃搭桥术(1842 [73.7%]),袖式胃切除术(381 [15.3%])。 ]),可调整的胃束带(249 [10.0%])和其他程序(26 [1.0%])。主要结果和措施本研究测量了总人数,门诊人数,住院人数,以及从手术前3年到手术后10年的门诊药房支出,不包括与初始减肥手术相关的支出。结果在9954名严重肥胖的退伍军人中,男性为7387名(74.2%)。手术队列的平均(SD)年龄为52.3(8.8)岁,非手术队列的平均(SD)年龄为52.5(8.7)岁。手术队列的平均总支出在手术前7到12个月为$ 5093(95%CI,$ 4811- $ 5391),在手术后6个月增加到$ 7448(95%CI,$ 6989- $ 7936)。术后5年的手术后支出降至$ 6692(95%CI,$ 6197- $ 7226),然后在术后10年逐渐增加到$ 8495(95%CI,$ 7609- $ 9484)。在手术前3年和手术后的前2年中,手术组的总支出高于非手术组。手术后5到10年,这两个队列的支出趋于一致。在所有随访期间,手术队列中的门诊药房支出均显着降低(术前3年降低509美元,术前7至12个月降低461美元),但住院和门诊费用的增加抵消了这些成本的降低(非药学) )支出。结论与相关性在这项队列研究中,对9954名主要患有严重肥胖症的男性老龄退伍军人进行了减肥手术后,其总医疗保健支出立即增加,但与那些在手术后10年未接受手术的患者的医疗支出相一致。
更新日期:2019-12-19
中文翻译:

肥胖症退伍军人中的减肥手术与长期医疗保健支出之间的关联。
重要性减肥手术已与重度肥胖患者的健康状况改善相关。但是,尚不清楚这些健康益处是否会转化为较低的医疗保健支出。目的在一项大型,多地点回顾性队列研究中,对接受过肥胖手术和不接受肥胖手术的退伍军人进行一项为期十年的大型回顾性队列研究,以研究其十年的医疗保健支出。设计,设置和参与者从退伍军人事务(VA)电子健康记录中识别出了2000年1月1日至2011年9月30日期间共有9954名严重肥胖的退伍军人。在这些人中,有2498名接受了减肥手术的退伍军人被分配到该手术队列中。依序进行分层,以使手术队列中的每位患者与最多3例未进行过减肥手术但性别相同的患者相匹配,种族/族裔,糖尿病状况和VA区域网络,并且年龄,体重指数(以体重(公斤)除以身高(米为平方)计算)和合并症最接近。总共确定了7456例患者,并将其分配到非手术(对照)队列中。使用回归模型估算了手术和非手术人群中的VA保健支出。分析了2018年7月至2018年8月以及2019年4月的数据。干预措施这项研究中包括的减肥手术方法(n = 2498)为Roux-en-Y胃搭桥术(1842 [73.7%]),袖式胃切除术(381 [15.3%])。 ]),可调整的胃束带(249 [10.0%])和其他程序(26 [1.0%])。主要结果和措施本研究测量了总人数,门诊人数,住院人数,以及从手术前3年到手术后10年的门诊药房支出,不包括与初始减肥手术相关的支出。结果在9954名严重肥胖的退伍军人中,男性为7387名(74.2%)。手术队列的平均(SD)年龄为52.3(8.8)岁,非手术队列的平均(SD)年龄为52.5(8.7)岁。手术队列的平均总支出在手术前7到12个月为$ 5093(95%CI,$ 4811- $ 5391),在手术后6个月增加到$ 7448(95%CI,$ 6989- $ 7936)。术后5年的手术后支出降至$ 6692(95%CI,$ 6197- $ 7226),然后在术后10年逐渐增加到$ 8495(95%CI,$ 7609- $ 9484)。在手术前3年和手术后的前2年中,手术组的总支出高于非手术组。手术后5到10年,这两个队列的支出趋于一致。在所有随访期间,手术队列中的门诊药房支出均显着降低(术前3年降低509美元,术前7至12个月降低461美元),但住院和门诊费用的增加抵消了这些成本的降低(非药学) )支出。结论与相关性在这项队列研究中,对9954名主要患有严重肥胖症的男性老龄退伍军人进行了减肥手术后,其总医疗保健支出立即增加,但与那些在手术后10年未接受手术的患者的医疗支出相一致。











































 京公网安备 11010802027423号
京公网安备 11010802027423号