当前位置:
X-MOL 学术
›
Lancet Infect Dis
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Quantifying risks and interventions that have affected the burden of lower respiratory infections among children younger than 5 years: an analysis for the Global Burden of Disease Study 2017.
The Lancet Infectious Diseases ( IF 36.4 ) Pub Date : 2019-10-31 , DOI: 10.1016/s1473-3099(19)30410-4 Christopher E Troeger , Ibrahim A Khalil , Brigette F Blacker , Molly H Biehl , Samuel B Albertson , Stephanie R M Zimsen , Puja C Rao , Degu Abate , Amha Admasie , Alireza Ahmadi , Mohamed Lemine Cheikh Brahim Ahmed , Chalachew Genet Akal , Fares Alahdab , Noore Alam , Kefyalew Addis Alene , Vahid Alipour , Syed Mohamed Aljunid , Rajaa M Al-Raddadi , Nelson Alvis-Guzman , Saeed Amini , Mina Anjomshoa , Carl Abelardo T Antonio , Jalal Arabloo , Olatunde Aremu , Hagos Tasew Atalay , Suleman Atique , Euripide F G A Avokpaho , Samah Awad , Ashish Awasthi , Alaa Badawi , Kalpana Balakrishnan , Joseph Adel Mattar Banoub , Aleksandra Barac , Quique Bassat , Neeraj Bedi , Derrick A Bennett , Krittika Bhattacharyya , Zulfiqar A Bhutta , Ali Bijani , Corey B Bills , Josip Car , Félix Carvalho , Carlos A Castañeda-Orjuela , Kate Causey , Devasahayam J Christopher , Aaron J Cohen , Lalit Dandona , Rakhi Dandona , Ahmad Daryani , Feleke Mekonnen Demeke , Shirin Djalalinia , Manisha Dubey , Eleonora Dubljanin , Eyasu Ejeta Duken , Maysaa El Sayed Zaki , Aman Yesuf Endries , Eduarda Fernandes , Florian Fischer , Joseph Frostad , Nancy Fullman , William M Gardner , Birhanu Geta , Keyghobad Ghadiri , Giuseppe Gorini , Alessandra C Goulart , Yuming Guo , Gessessew Bugssa Hailu , Arvin Haj-Mirzaian , Arya Haj-Mirzaian , Samer Hamidi , Hamid Yimam Hassen , Chi Linh Hoang , Nobuyuki Horita , Mihaela Hostiuc , Zakir Hussain , Seyed Sina Naghibi Irvani , Spencer L James , Ravi Prakash Jha , Jost B Jonas , André Karch , Amir Kasaeian , Tesfaye Dessale Kassa , Nicholas J Kassebaum , Adane Teshome Kefale , Yousef Saleh Khader , Ejaz Ahmad Khan , Gulfaraz Khan , Md Nuruzzaman Khan , Young-Ho Khang , Abdullah T Khoja , Ruth W Kimokoti , Adnan Kisa , Sezer Kisa , Niranjan Kissoon , Luke D Knibbs , Sonali Kochhar , Soewarta Kosen , Parvaiz A Koul , Ai Koyanagi , Barthelemy Kuate Defo , G Anil Kumar , Dharmesh Kumar Lal , Cheru Tesema Leshargie , Sonia Lewycka , Shanshan Li , Rakesh Lodha , Erlyn Rachelle King Macarayan , Marek Majdan , Abdullah A Mamun , Helena Manguerra , Varshil Mehta , Addisu Melese , Ziad A Memish , Desalegn Tadese Mengistu , Tuomo J Meretoja , Tomislav Mestrovic , Bartosz Miazgowski , Erkin M Mirrakhimov , Babak Moazen , Karzan Abdulmuhsin Mohammad , Shafiu Mohammed , Lorenzo Monasta , Catrin E Moore , Lidia Morawska , Jonathan F Mosser , Seyyed Meysam Mousavi , Srinivas Murthy , Ghulam Mustafa , Javad Nazari , Cuong Tat Nguyen , Huong Lan Thi Nguyen , Long Hoang Nguyen , Son Hoang Nguyen , Katie R Nielsen , Muhammad Imran Nisar , Molly R Nixon , Felix Akpojene Ogbo , Anselm Okoro , Andrew T Olagunju , Tinuke O Olagunju , Eyal Oren , Justin R Ortiz , Mahesh P A , Smita Pakhale , Maarten J Postma , Mostafa Qorbani , Reginald Quansah , Alireza Rafiei , Fakher Rahim , Vafa Rahimi-Movaghar , Rajesh Kumar Rai , Marissa Bettay Reitsma , Mohammad Sadegh Rezai , Aziz Rezapour , Maria Jesus Rios-Blancas , Luca Ronfani , Dietrich Rothenbacher , Salvatore Rubino , Zikria Saleem , Evanson Zondani Sambala , Abdallah M Samy , Milena M Santric Milicevic , Rodrigo Sarmiento-Suárez , Benn Sartorius , Miloje Savic , Monika Sawhney , Sonia Saxena , Alyssa Sbarra , Seyedmojtaba Seyedmousavi , Masood Ali Shaikh , Aziz Sheikh , Mika Shigematsu , David L Smith , Chandrashekhar T Sreeramareddy , Jeffrey D Stanaway , Mu'awiyyah Babale Sufiyan , Mohamad-Hani Temsah , Belay Tessema , Bach Xuan Tran , Khanh Bao Tran , Afewerki Gebremeskel Tsadik , Irfan Ullah , Rachel L Updike , Tommi Juhani Vasankari , Yousef Veisani , Fiseha Wadilo Wada , Yasir Waheed , Katie Welgan , Kirsten E Wiens , Charles Shey Wiysonge , Ebrahim M Yimer , Naohiro Yonemoto , Zoubida Zaidi , Heather J Zar , Stephen S Lim , Theo Vos , Ali H Mokdad , Christopher J L Murray , Hmwe Hmwe Kyu , Simon I Hay , Robert C Reiner
The Lancet Infectious Diseases ( IF 36.4 ) Pub Date : 2019-10-31 , DOI: 10.1016/s1473-3099(19)30410-4 Christopher E Troeger , Ibrahim A Khalil , Brigette F Blacker , Molly H Biehl , Samuel B Albertson , Stephanie R M Zimsen , Puja C Rao , Degu Abate , Amha Admasie , Alireza Ahmadi , Mohamed Lemine Cheikh Brahim Ahmed , Chalachew Genet Akal , Fares Alahdab , Noore Alam , Kefyalew Addis Alene , Vahid Alipour , Syed Mohamed Aljunid , Rajaa M Al-Raddadi , Nelson Alvis-Guzman , Saeed Amini , Mina Anjomshoa , Carl Abelardo T Antonio , Jalal Arabloo , Olatunde Aremu , Hagos Tasew Atalay , Suleman Atique , Euripide F G A Avokpaho , Samah Awad , Ashish Awasthi , Alaa Badawi , Kalpana Balakrishnan , Joseph Adel Mattar Banoub , Aleksandra Barac , Quique Bassat , Neeraj Bedi , Derrick A Bennett , Krittika Bhattacharyya , Zulfiqar A Bhutta , Ali Bijani , Corey B Bills , Josip Car , Félix Carvalho , Carlos A Castañeda-Orjuela , Kate Causey , Devasahayam J Christopher , Aaron J Cohen , Lalit Dandona , Rakhi Dandona , Ahmad Daryani , Feleke Mekonnen Demeke , Shirin Djalalinia , Manisha Dubey , Eleonora Dubljanin , Eyasu Ejeta Duken , Maysaa El Sayed Zaki , Aman Yesuf Endries , Eduarda Fernandes , Florian Fischer , Joseph Frostad , Nancy Fullman , William M Gardner , Birhanu Geta , Keyghobad Ghadiri , Giuseppe Gorini , Alessandra C Goulart , Yuming Guo , Gessessew Bugssa Hailu , Arvin Haj-Mirzaian , Arya Haj-Mirzaian , Samer Hamidi , Hamid Yimam Hassen , Chi Linh Hoang , Nobuyuki Horita , Mihaela Hostiuc , Zakir Hussain , Seyed Sina Naghibi Irvani , Spencer L James , Ravi Prakash Jha , Jost B Jonas , André Karch , Amir Kasaeian , Tesfaye Dessale Kassa , Nicholas J Kassebaum , Adane Teshome Kefale , Yousef Saleh Khader , Ejaz Ahmad Khan , Gulfaraz Khan , Md Nuruzzaman Khan , Young-Ho Khang , Abdullah T Khoja , Ruth W Kimokoti , Adnan Kisa , Sezer Kisa , Niranjan Kissoon , Luke D Knibbs , Sonali Kochhar , Soewarta Kosen , Parvaiz A Koul , Ai Koyanagi , Barthelemy Kuate Defo , G Anil Kumar , Dharmesh Kumar Lal , Cheru Tesema Leshargie , Sonia Lewycka , Shanshan Li , Rakesh Lodha , Erlyn Rachelle King Macarayan , Marek Majdan , Abdullah A Mamun , Helena Manguerra , Varshil Mehta , Addisu Melese , Ziad A Memish , Desalegn Tadese Mengistu , Tuomo J Meretoja , Tomislav Mestrovic , Bartosz Miazgowski , Erkin M Mirrakhimov , Babak Moazen , Karzan Abdulmuhsin Mohammad , Shafiu Mohammed , Lorenzo Monasta , Catrin E Moore , Lidia Morawska , Jonathan F Mosser , Seyyed Meysam Mousavi , Srinivas Murthy , Ghulam Mustafa , Javad Nazari , Cuong Tat Nguyen , Huong Lan Thi Nguyen , Long Hoang Nguyen , Son Hoang Nguyen , Katie R Nielsen , Muhammad Imran Nisar , Molly R Nixon , Felix Akpojene Ogbo , Anselm Okoro , Andrew T Olagunju , Tinuke O Olagunju , Eyal Oren , Justin R Ortiz , Mahesh P A , Smita Pakhale , Maarten J Postma , Mostafa Qorbani , Reginald Quansah , Alireza Rafiei , Fakher Rahim , Vafa Rahimi-Movaghar , Rajesh Kumar Rai , Marissa Bettay Reitsma , Mohammad Sadegh Rezai , Aziz Rezapour , Maria Jesus Rios-Blancas , Luca Ronfani , Dietrich Rothenbacher , Salvatore Rubino , Zikria Saleem , Evanson Zondani Sambala , Abdallah M Samy , Milena M Santric Milicevic , Rodrigo Sarmiento-Suárez , Benn Sartorius , Miloje Savic , Monika Sawhney , Sonia Saxena , Alyssa Sbarra , Seyedmojtaba Seyedmousavi , Masood Ali Shaikh , Aziz Sheikh , Mika Shigematsu , David L Smith , Chandrashekhar T Sreeramareddy , Jeffrey D Stanaway , Mu'awiyyah Babale Sufiyan , Mohamad-Hani Temsah , Belay Tessema , Bach Xuan Tran , Khanh Bao Tran , Afewerki Gebremeskel Tsadik , Irfan Ullah , Rachel L Updike , Tommi Juhani Vasankari , Yousef Veisani , Fiseha Wadilo Wada , Yasir Waheed , Katie Welgan , Kirsten E Wiens , Charles Shey Wiysonge , Ebrahim M Yimer , Naohiro Yonemoto , Zoubida Zaidi , Heather J Zar , Stephen S Lim , Theo Vos , Ali H Mokdad , Christopher J L Murray , Hmwe Hmwe Kyu , Simon I Hay , Robert C Reiner
|
BACKGROUND
Despite large reductions in under-5 lower respiratory infection (LRI) mortality in many locations, the pace of progress for LRIs has generally lagged behind that of other childhood infectious diseases. To better inform programmes and policies focused on preventing and treating LRIs, we assessed the contributions and patterns of risk factor attribution, intervention coverage, and sociodemographic development in 195 countries and territories by drawing from the Global Burden of Diseases, Injuries, and Risk Factors Study 2017 (GBD 2017) LRI estimates.
METHODS
We used four strategies to model LRI burden: the mortality due to LRIs was modelled using vital registration data, demographic surveillance data, and verbal autopsy data in a predictive ensemble modelling tool; the incidence of LRIs was modelled using population representative surveys, health-care utilisation data, and scientific literature in a compartmental meta-regression tool; the attribution of risk factors for LRI mortality was modelled in a counterfactual framework; and trends in LRI mortality were analysed applying changes in exposure to risk factors over time. In GBD, infectious disease mortality, including that due to LRI, is among HIV-negative individuals. We categorised locations based on their burden in 1990 to make comparisons in the changing burden between 1990 and 2017 and evaluate the relative percent change in mortality rate, incidence, and risk factor exposure to explain differences in the health loss associated with LRIs among children younger than 5 years.
FINDINGS
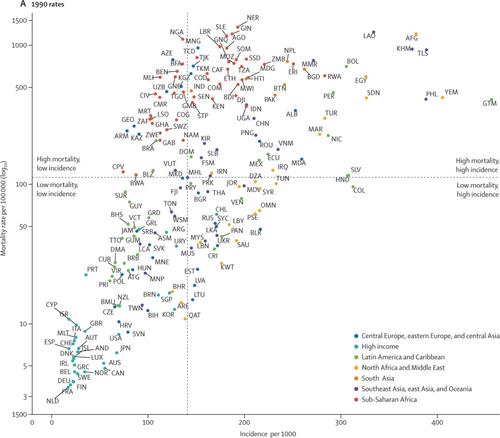
In 2017, LRIs caused 808 920 deaths (95% uncertainty interval 747 286-873 591) in children younger than 5 years. Since 1990, there has been a substantial decrease in the number of deaths (from 2 337 538 to 808 920 deaths; 65·4% decrease, 61·5-68·5) and in mortality rate (from 362·7 deaths [330·1-392·0] per 100 000 children to 118·9 deaths [109·8-128·3] per 100 000 children; 67·2% decrease, 63·5-70·1). LRI incidence declined globally (32·4% decrease, 27·2-37·5). The percent change in under-5 mortality rate and incidence has varied across locations. Among the risk factors assessed in this study, those responsible for the greatest decrease in under-5 LRI mortality between 1990 and 2017 were increased coverage of vaccination against Haemophilus influenza type b (11·4% decrease, 0·0-24·5), increased pneumococcal vaccine coverage (6·3% decrease, 6·1-6·3), and reductions in household air pollution (8·4%, 6·8-9·2).
INTERPRETATION
Our findings show that there have been substantial but uneven declines in LRI mortality among countries between 1990 and 2017. Although improvements in indicators of sociodemographic development could explain some of these trends, changes in exposure to modifiable risk factors are related to the rates of decline in LRI mortality. No single intervention would universally accelerate reductions in health loss associated with LRIs in all settings, but emphasising the most dominant risk factors, particularly in countries with high case fatality, can contribute to the reduction of preventable deaths.
FUNDING
Bill & Melinda Gates Foundation.
中文翻译:

量化影响5岁以下儿童下呼吸道感染负担的风险和干预措施:《 2017年全球疾病负担研究》的一项分析。
背景技术尽管在许多地方大大降低了5岁以下下呼吸道感染(LRI)的死亡率,但是LRI的发展步伐通常落后于其他儿童传染病的步伐。为了更好地宣传旨在预防和治疗LRI的计划和政策,我们从全球疾病,伤害和风险因素研究中评估了195个国家和地区的风险因素归因,干预范围以及社会人口学发展的贡献和模式。 2017年(GBD 2017)LRI估算。方法我们采用了四种策略对LRI负荷进行建模:在可预测的整体建模工具中,使用生命登记数据,人口统计数据和口头尸检数据对LRI造成的死亡率进行建模。LRIs的发生率是使用人群代表性调查,卫生保健利用数据和科学文献在隔间元回归工具中建模的;LRI死亡率的危险因素的归因是在反事实框架中建模的;并分析了LRI死亡率的趋势,方法是随着时间推移暴露于危险因素的变化。在GBD中,包括HIV阴性在内的传染病死亡率,包括LRI引起的死亡率。我们根据1990年的负担对地点进行了分类,以比较1990年至2017年间不断变化的负担,并评估死亡率,发病率和危险因素暴露的相对百分比变化,以解释年龄小于1岁的儿童与LRI相关的健康损失的差异5年。调查结果2017年,LRI在5岁以下的儿童中造成808,920例死亡(95%不确定区间747 286-873 591)。自1990年以来,死亡人数(从2 337 538减少到808 920;减少了65·4%,分别是61·5-68·5)和死亡率(从362·7死亡[330]每10万名儿童·1-392·0],每10万名儿童有118·9死亡[109·8-128·3];减少67·2%,63·5-70·1)。全球LRI发病率下降(下降32·4%,下降27·2-37·5)。5岁以下儿童死亡率和发生率的百分比变化在各个地区都不同。在本研究评估的风险因素中,1990年至2017年期间导致5岁以下LRI死亡率下降最多的因素是接种乙型流感嗜血杆菌疫苗的覆盖面增加(下降11·4%,0·0-24·5) ,肺炎球菌疫苗覆盖率增加(减少6·3%,减少6·1-6·3),减少家庭空气污染(8·4%,6·8-9·2)。解释我们的研究结果表明,1990年至2017年间,各国的LRI死亡率有大幅下降但不均衡。尽管社会人口发展指标的改善可以解释其中的一些趋势,但可调整的风险因素暴露的变化与下降率有关在LRI死亡率方面。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。解释我们的研究结果表明,1990年至2017年间,各国的LRI死亡率有大幅下降但不均衡。尽管社会人口发展指标的改善可以解释其中的一些趋势,但可调整的风险因素暴露的变化与下降率有关在LRI死亡率方面。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。解释我们的研究结果表明,1990年至2017年间,各国的LRI死亡率有大幅下降但不均衡。尽管社会人口发展指标的改善可以解释其中的一些趋势,但可调整的风险因素暴露的变化与下降率有关在LRI死亡率方面。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。暴露于可改变的危险因素中的变化与LRI死亡率下降的速率有关。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。暴露于可改变的危险因素中的变化与LRI死亡率下降的速率有关。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。
更新日期:2019-12-25
中文翻译:

量化影响5岁以下儿童下呼吸道感染负担的风险和干预措施:《 2017年全球疾病负担研究》的一项分析。
背景技术尽管在许多地方大大降低了5岁以下下呼吸道感染(LRI)的死亡率,但是LRI的发展步伐通常落后于其他儿童传染病的步伐。为了更好地宣传旨在预防和治疗LRI的计划和政策,我们从全球疾病,伤害和风险因素研究中评估了195个国家和地区的风险因素归因,干预范围以及社会人口学发展的贡献和模式。 2017年(GBD 2017)LRI估算。方法我们采用了四种策略对LRI负荷进行建模:在可预测的整体建模工具中,使用生命登记数据,人口统计数据和口头尸检数据对LRI造成的死亡率进行建模。LRIs的发生率是使用人群代表性调查,卫生保健利用数据和科学文献在隔间元回归工具中建模的;LRI死亡率的危险因素的归因是在反事实框架中建模的;并分析了LRI死亡率的趋势,方法是随着时间推移暴露于危险因素的变化。在GBD中,包括HIV阴性在内的传染病死亡率,包括LRI引起的死亡率。我们根据1990年的负担对地点进行了分类,以比较1990年至2017年间不断变化的负担,并评估死亡率,发病率和危险因素暴露的相对百分比变化,以解释年龄小于1岁的儿童与LRI相关的健康损失的差异5年。调查结果2017年,LRI在5岁以下的儿童中造成808,920例死亡(95%不确定区间747 286-873 591)。自1990年以来,死亡人数(从2 337 538减少到808 920;减少了65·4%,分别是61·5-68·5)和死亡率(从362·7死亡[330]每10万名儿童·1-392·0],每10万名儿童有118·9死亡[109·8-128·3];减少67·2%,63·5-70·1)。全球LRI发病率下降(下降32·4%,下降27·2-37·5)。5岁以下儿童死亡率和发生率的百分比变化在各个地区都不同。在本研究评估的风险因素中,1990年至2017年期间导致5岁以下LRI死亡率下降最多的因素是接种乙型流感嗜血杆菌疫苗的覆盖面增加(下降11·4%,0·0-24·5) ,肺炎球菌疫苗覆盖率增加(减少6·3%,减少6·1-6·3),减少家庭空气污染(8·4%,6·8-9·2)。解释我们的研究结果表明,1990年至2017年间,各国的LRI死亡率有大幅下降但不均衡。尽管社会人口发展指标的改善可以解释其中的一些趋势,但可调整的风险因素暴露的变化与下降率有关在LRI死亡率方面。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。解释我们的研究结果表明,1990年至2017年间,各国的LRI死亡率有大幅下降但不均衡。尽管社会人口发展指标的改善可以解释其中的一些趋势,但可调整的风险因素暴露的变化与下降率有关在LRI死亡率方面。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。解释我们的研究结果表明,1990年至2017年间,各国的LRI死亡率有大幅下降但不均衡。尽管社会人口发展指标的改善可以解释其中的一些趋势,但可调整的风险因素暴露的变化与下降率有关在LRI死亡率方面。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。暴露于可改变的危险因素中的变化与LRI死亡率下降的速率有关。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。暴露于可改变的危险因素中的变化与LRI死亡率下降的速率有关。在所有情况下,没有任何一种干预措施能够普遍加速减少与LRI相关的健康损失,但是强调最主要的危险因素,尤其是在高病死率国家中,可以有助于减少可预防的死亡。资金比尔和梅琳达·盖茨基金会。











































 京公网安备 11010802027423号
京公网安备 11010802027423号