当前位置:
X-MOL 学术
›
Acta Pharm. Sin. B
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Abnormal metabolism of gut microbiota reveals the possible molecular mechanism of nephropathy induced by hyperuricemia.
Acta Pharmaceutica Sinica B ( IF 14.7 ) Pub Date : 2019-10-30 , DOI: 10.1016/j.apsb.2019.10.007 Libin Pan 1 , Pei Han 1 , Shurong Ma 1 , Ran Peng 1 , Can Wang 1 , Weijia Kong 2 , Lin Cong 1 , Jie Fu 1 , Zhengwei Zhang 1 , Hang Yu 1 , Yan Wang 1 , Jiandong Jiang 1
Acta Pharmaceutica Sinica B ( IF 14.7 ) Pub Date : 2019-10-30 , DOI: 10.1016/j.apsb.2019.10.007 Libin Pan 1 , Pei Han 1 , Shurong Ma 1 , Ran Peng 1 , Can Wang 1 , Weijia Kong 2 , Lin Cong 1 , Jie Fu 1 , Zhengwei Zhang 1 , Hang Yu 1 , Yan Wang 1 , Jiandong Jiang 1
Affiliation
|
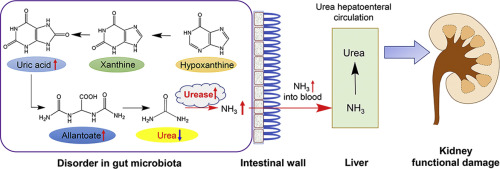
The progression of hyperuricemia disease is often accompanied by damage to renal function. However, there are few studies on hyperuricemia nephropathy, especially its association with intestinal flora. This study combines metabolomics and gut microbiota diversity analysis to explore metabolic changes using a rat model as well as the changes in intestinal flora composition. The results showed that amino acid metabolism was disturbed with serine, glutamate and glutamine being downregulated whilst glycine, hydroxyproline and alanine being upregulated. The combined glycine, serine and glutamate could predict hyperuricemia nephropathy with an area under the curve of 1.00. Imbalanced intestinal flora was also observed. Flavobacterium, Myroides, Corynebacterium, Alcaligenaceae, Oligella and other conditional pathogens increased significantly in the model group, while Blautia and Roseburia, the short-chain fatty acid producing bacteria, declined greatly. At phylum, family and genus levels, disordered nitrogen circulation in gut microbiota was detected. In the model group, the uric acid decomposition pathway was enhanced with reinforced urea liver-intestine circulation. The results implied that the intestinal flora play a vital role in the pathogenesis of hyperuricemia nephropathy. Hence, modulation of gut microbiota or targeting at metabolic enzymes, i.e., urease, could assist the treatment and prevention of this disease.
中文翻译:

肠道菌群的新陈代谢异常揭示了高尿酸血症所致肾病的可能分子机制。
高尿酸血症疾病的进展通常伴随着肾功能的损害。然而,关于高尿酸血症肾病,特别是其与肠道菌群的关系的研究很少。这项研究结合了代谢组学和肠道菌群多样性分析,以探索使用大鼠模型的代谢变化以及肠道菌群组成的变化。结果表明,丝氨酸,谷氨酸和谷氨酰胺被下调而甘氨酸,羟脯氨酸和丙氨酸被上调干扰氨基酸代谢。甘氨酸,丝氨酸和谷氨酸的组合可以预测高尿酸血症性肾病,其面积在1.00以下。还观察到肠道菌群失衡。黄杆菌,类固醇,棒状杆菌,拟南芥科,在模型组中,小球藻和其他条件性病原体显着增加,而短链脂肪酸产生菌Blautia和Roseburia则大大减少。在门,科和属水平上,检测到肠道菌群中氮循环异常。在模型组中,尿素肝肠循环的增强增强了尿酸的分解途径。结果表明,肠道菌群在高尿酸血症肾病的发病机理中起着至关重要的作用。因此,调节肠道菌群或靶向代谢酶即脲酶可以帮助治疗和预防这种疾病。在模型组中,尿素肝肠循环的增强增强了尿酸的分解途径。结果表明,肠道菌群在高尿酸血症肾病的发病机理中起着至关重要的作用。因此,调节肠道菌群或靶向代谢酶即脲酶可以帮助治疗和预防这种疾病。在模型组中,尿素肝肠循环的增强增强了尿酸的分解途径。结果表明,肠道菌群在高尿酸血症肾病的发病机理中起着至关重要的作用。因此,调节肠道菌群或靶向代谢酶即脲酶可以帮助治疗和预防这种疾病。
更新日期:2019-11-01
中文翻译:

肠道菌群的新陈代谢异常揭示了高尿酸血症所致肾病的可能分子机制。
高尿酸血症疾病的进展通常伴随着肾功能的损害。然而,关于高尿酸血症肾病,特别是其与肠道菌群的关系的研究很少。这项研究结合了代谢组学和肠道菌群多样性分析,以探索使用大鼠模型的代谢变化以及肠道菌群组成的变化。结果表明,丝氨酸,谷氨酸和谷氨酰胺被下调而甘氨酸,羟脯氨酸和丙氨酸被上调干扰氨基酸代谢。甘氨酸,丝氨酸和谷氨酸的组合可以预测高尿酸血症性肾病,其面积在1.00以下。还观察到肠道菌群失衡。黄杆菌,类固醇,棒状杆菌,拟南芥科,在模型组中,小球藻和其他条件性病原体显着增加,而短链脂肪酸产生菌Blautia和Roseburia则大大减少。在门,科和属水平上,检测到肠道菌群中氮循环异常。在模型组中,尿素肝肠循环的增强增强了尿酸的分解途径。结果表明,肠道菌群在高尿酸血症肾病的发病机理中起着至关重要的作用。因此,调节肠道菌群或靶向代谢酶即脲酶可以帮助治疗和预防这种疾病。在模型组中,尿素肝肠循环的增强增强了尿酸的分解途径。结果表明,肠道菌群在高尿酸血症肾病的发病机理中起着至关重要的作用。因此,调节肠道菌群或靶向代谢酶即脲酶可以帮助治疗和预防这种疾病。在模型组中,尿素肝肠循环的增强增强了尿酸的分解途径。结果表明,肠道菌群在高尿酸血症肾病的发病机理中起着至关重要的作用。因此,调节肠道菌群或靶向代谢酶即脲酶可以帮助治疗和预防这种疾病。











































 京公网安备 11010802027423号
京公网安备 11010802027423号