当前位置:
X-MOL 学术
›
Lancet Infect Dis
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Long-term survival and cause-specific mortality of patients newly diagnosed with tuberculosis in São Paulo state, Brazil, 2010-15: a population-based, longitudinal study.
The Lancet Infectious Diseases ( IF 36.4 ) Pub Date : 2019-10-31 , DOI: 10.1016/s1473-3099(19)30518-3 Otavio T Ranzani 1 , Laura C Rodrigues 2 , Sidney Bombarda 3 , Cátia M Minto 4 , Eliseu A Waldman 5 , Carlos R R Carvalho 6
The Lancet Infectious Diseases ( IF 36.4 ) Pub Date : 2019-10-31 , DOI: 10.1016/s1473-3099(19)30518-3 Otavio T Ranzani 1 , Laura C Rodrigues 2 , Sidney Bombarda 3 , Cátia M Minto 4 , Eliseu A Waldman 5 , Carlos R R Carvalho 6
Affiliation
|
BACKGROUND
Long-term survival and cause-specific mortality of patients who start tuberculosis treatment is rarely described. We aimed to assess the long-term survival of these patients and evaluate the association between vulnerable conditions (social, health behaviours, and comorbidities) and cause-specific mortality in a country with a high burden of tuberculosis.
METHODS
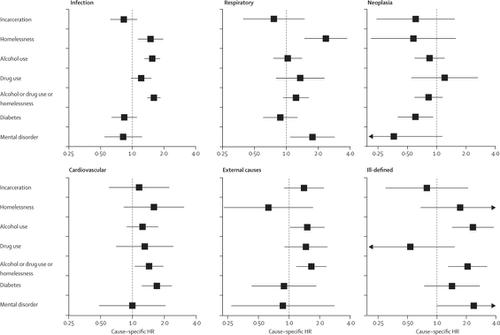
In this population-based, longitudinal study in São Paulo state, Brazil, we described the 5-year survival of patients who were newly diagnosed with tuberculosis in 2010. We included patients with newly-diagnosed tuberculosis, aged 15 years or older, and notified to the São Paulo State Tuberculosis Program in 2010. We excluded patients whose diagnosis had changed during follow-up (ie, they did not have tuberculosis) and patients who had multidrug-resistant (MDR) tuberculosis. We selected our population with tuberculosis from the dedicated electronic system TBweb. Our primary objective was to estimate the excess mortality over 5 years and within the group who survived the first year, compared with the general São Paulo state population. We also estimated the association between social vulnerability (imprisonment and homelessness), health behaviours (alcohol and drug use), and comorbidities (diabetes and mental disorders) with all-cause and cause-specific mortality. We used the competing risk analysis framework, estimating cause-specific hazard ratios (HRs) adjusted for potential confounding factors.
FINDINGS
In 2010, there were 19 252 notifications of tuberculosis cases. We excluded 550 cases as patients were younger than 15 years, 556 cases that were not tuberculosis, 2597 retreatments, and 48 cases of MDR tuberculosis, resulting in a final cohort of 15 501 patients with tuberculosis. Over a period of 5 years from tuberculosis diagnosis, 2660 (17%) of 15 501 patients died. Compared with the source population, matched by age, sex, and calendar year, the standardised mortality ratio was 6·47 (95% CI 6·22-6·73) over 5 years and 3·93 (3·71-4·17) among those who survived the first year. 1197 (45%) of 2660 deaths were due to infection. Homelessness and alcohol and drug use were associated with death from infection (adjusted cause-specific HR 1·60, 95% CI 1·39-1·85), cardiovascular (1·43, 1·06-1·95), and external or ill-defined causes of death (1·80, 1·37-2·36). Diabetes was associated with deaths from cardiovascular causes (1·70, 1·23-2·35).
INTERPRETATION
Patients newly diagnosed with tuberculosis were at a higher risk of death than were the source population, even after tuberculosis treatment. Post-tuberculosis sequelae and vulnerability are associated with excess mortality and must be addressed to mitigate the tuberculosis burden worldwide.
FUNDING
Wellcome Trust.
中文翻译:

2010-15 年巴西圣保罗州新诊断结核病患者的长期生存率和特定原因死亡率:一项基于人群的纵向研究。
背景 开始结核病治疗的患者的长期生存率和特定原因死亡率很少被描述。我们的目的是评估这些患者的长期生存率,并评估结核病高负担国家的脆弱状况(社会、健康行为和合并症)与特定原因死亡率之间的关联。方法 在巴西圣保罗州这项基于人群的纵向研究中,我们描述了 2010 年新诊断结核病患者的 5 年生存率。我们纳入了新诊断结核病患者,年龄为 15 岁或以上, 2010 年向圣保罗州结核病规划通报。我们排除了在随访期间诊断发生变化的患者(即他们没有患有结核病)和患有耐多药 (MDR) 结核病的患者。我们从专用电子系统 TBweb 中选择了患有结核病的人群。我们的主要目标是与圣保罗州总人口相比,估算 5 年内以及第一年存活群体内的超额死亡率。我们还估计了社会脆弱性(监禁和无家可归)、健康行为(酗酒和吸毒)以及合并症(糖尿病和精神障碍)与全因和特定原因死亡率之间的关联。我们使用竞争风险分析框架,估计针对潜在混杂因素进行调整的特定原因风险比(HR)。结果 2010 年,共通报了 19 252 例肺结核病例。我们排除了 550 例年龄小于 15 岁的患者、556 例非结核病患者、2597 例复治患者和 48 例耐多药结核病患者,最终得到 15 501 例结核病患者。 结核病诊断后 5 年内,15 501 名患者中有 2 660 名患者(17%)死亡。与源人群相比,按年龄、性别和历年匹配,5年内标准化死亡率为6·47 (95% CI 6·22-6·73),5年内标准化死亡率为3·93 (3·71-4· 17)在第一年幸存的人中。 2660 例死亡中有 1197 例(45%)是由于感染造成的。无家可归、酗酒和吸毒与感染死亡(调整后的具体原因 HR 1·60,95% CI 1·39-1·85)、心血管疾病(1·43、1·06-1·95)和外部或不明确的死亡原因(1·80、1·37-2·36)。糖尿病与心血管原因死亡相关 (1·70, 1·23-2·35)。解释 新诊断结核病患者的死亡风险高于来源人群,即使在结核病治疗后也是如此。结核病后遗症和脆弱性与死亡率过高有关,必须加以解决,以减轻全世界的结核病负担。资助威康信托。
更新日期:2019-12-25
中文翻译:

2010-15 年巴西圣保罗州新诊断结核病患者的长期生存率和特定原因死亡率:一项基于人群的纵向研究。
背景 开始结核病治疗的患者的长期生存率和特定原因死亡率很少被描述。我们的目的是评估这些患者的长期生存率,并评估结核病高负担国家的脆弱状况(社会、健康行为和合并症)与特定原因死亡率之间的关联。方法 在巴西圣保罗州这项基于人群的纵向研究中,我们描述了 2010 年新诊断结核病患者的 5 年生存率。我们纳入了新诊断结核病患者,年龄为 15 岁或以上, 2010 年向圣保罗州结核病规划通报。我们排除了在随访期间诊断发生变化的患者(即他们没有患有结核病)和患有耐多药 (MDR) 结核病的患者。我们从专用电子系统 TBweb 中选择了患有结核病的人群。我们的主要目标是与圣保罗州总人口相比,估算 5 年内以及第一年存活群体内的超额死亡率。我们还估计了社会脆弱性(监禁和无家可归)、健康行为(酗酒和吸毒)以及合并症(糖尿病和精神障碍)与全因和特定原因死亡率之间的关联。我们使用竞争风险分析框架,估计针对潜在混杂因素进行调整的特定原因风险比(HR)。结果 2010 年,共通报了 19 252 例肺结核病例。我们排除了 550 例年龄小于 15 岁的患者、556 例非结核病患者、2597 例复治患者和 48 例耐多药结核病患者,最终得到 15 501 例结核病患者。 结核病诊断后 5 年内,15 501 名患者中有 2 660 名患者(17%)死亡。与源人群相比,按年龄、性别和历年匹配,5年内标准化死亡率为6·47 (95% CI 6·22-6·73),5年内标准化死亡率为3·93 (3·71-4· 17)在第一年幸存的人中。 2660 例死亡中有 1197 例(45%)是由于感染造成的。无家可归、酗酒和吸毒与感染死亡(调整后的具体原因 HR 1·60,95% CI 1·39-1·85)、心血管疾病(1·43、1·06-1·95)和外部或不明确的死亡原因(1·80、1·37-2·36)。糖尿病与心血管原因死亡相关 (1·70, 1·23-2·35)。解释 新诊断结核病患者的死亡风险高于来源人群,即使在结核病治疗后也是如此。结核病后遗症和脆弱性与死亡率过高有关,必须加以解决,以减轻全世界的结核病负担。资助威康信托。











































 京公网安备 11010802027423号
京公网安备 11010802027423号