JAMA Neurology ( IF 20.4 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamaneurol.2019.3403 Peter B Sporns 1 , Ronald Sträter 2 , Jens Minnerup 3 , Heinz Wiendl 3 , Uta Hanning 4 , René Chapot 5 , Hans Henkes 6 , Elina Henkes 6 , Astrid Grams 7 , Franziska Dorn 8 , Omid Nikoubashman 9 , Martin Wiesmann 9 , Georg Bier 1, 10 , Anushe Weber 11 , Gabriel Broocks 4 , Jens Fiehler 4 , Alex Brehm 12 , Marios Psychogios 12 , Daniel Kaiser 13 , Umut Yilmaz 14 , Andrea Morotti 15 , Wolfgang Marik 16 , Richard Nolz 17 , Ulf Jensen-Kondering 18 , Bernd Schmitz 19 , Stefan Schob 20 , Oliver Beuing 21 , Friedrich Götz 22 , Johannes Trenkler 23 , Bernd Turowski 24 , Markus Möhlenbruch 25 , Christina Wendl 26 , Peter Schramm 27 , Patricia Musolino 28 , Sarah Lee 29 , Marc Schlamann 30 , Alexander Radbruch 31 , Nicole Rübsamen 32 , André Karch 32 , Walter Heindel 1 , Moritz Wildgruber 1 , André Kemmling 3
|
Importance Randomized clinical trials have shown the efficacy of thrombectomy of large intracranial vessel occlusions in adults; however, any association of therapy with clinical outcomes in children is unknown.
Objective To evaluate the use of endovascular recanalization in pediatric patients with arterial ischemic stroke.
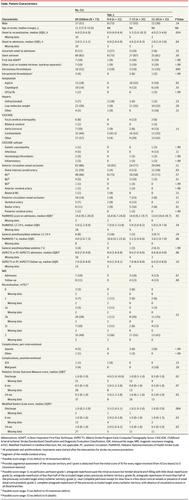
Design, Setting, and Participants This retrospective, multicenter cohort study, conducted from January 1, 2000, to December 31, 2018, analyzed the databases from 27 stroke centers in Europe and the United States. Included were all pediatric patients (<18 years) with ischemic stroke who underwent endovascular recanalization. Median follow-up time was 16 months.
Exposures Endovascular recanalization.
Main Outcomes and Measures The decrease of the Pediatric National Institutes of Health Stroke Scale (PedNIHSS) score from admission to day 7 was the primary outcome (score range: 0 [no deficit] to 34 [maximum deficit]). Secondary clinical outcomes included the modified Rankin scale (mRS) (score range: 0 [no deficit] to 6 [death]) at 6 and 24 months and rate of complications.
Results Seventy-three children from 27 participating stroke centers were included. Median age was 11.3 years (interquartile range [IQR], 7.0-15.0); 37 patients (51%) were boys, and 36 patients (49%) were girls. Sixty-three children (86%) received treatment for anterior circulation occlusion and 10 patients (14%) received treatment for posterior circulation occlusion; 16 patients (22%) received concomitant intravenous thrombolysis. Neurologic outcome improved from a median PedNIHSS score of 14.0 (IQR, 9.2-20.0) at admission to 4.0 (IQR, 2.0-7.3) at day 7. Median mRS score was 1.0 (IQR, 0-1.6) at 6 months and 1.0 (IQR, 0-1.0) at 24 months. One patient (1%) developed a postinterventional bleeding complication and 4 patients (5%) developed transient peri-interventional vasospasm. The proportion of symptomatic intracerebral hemorrhage events in the HERMES meta-analysis of trials with adults was 2.79 (95% CI, 0.42-6.66) and in Save ChildS was 1.37 (95% CI, 0.03-7.40).
Conclusions and Relevance The results of this study suggest that the safety profile of thrombectomy in childhood stroke does not differ from the safety profile in randomized clinical trials for adults; most of the treated children had favorable neurologic outcomes. This study may support clinicians’ practice of off-label thrombectomy in childhood stroke in the absence of high-level evidence.
中文翻译:

儿童中风后血管再通的可行性,安全性和结果:Save ChildS研究。
重要性 随机临床试验显示了成人大颅内血管闭塞的血栓切除术的有效性。然而,治疗与儿童临床结局的任何关联均未知。
目的 评估血管内再通技术在小儿动脉缺血性卒中患者中的应用。
设计,设置和参与者 这项回顾性,多中心队列研究于2000年1月1日至2018年12月31日进行,分析了来自欧洲和美国27个卒中中心的数据库。包括所有接受过血管内再通的缺血性卒中的小儿患者(<18岁)。中位随访时间为16个月。
暴露 血管内再通。
主要结果和措施 从入院到第7天儿童国立卫生研究院卒中量表(PedNIHSS)得分的降低是主要结局(评分范围:0 [无赤字]至34 [最大赤字])。次要临床结果包括改良的Rankin量表(mRS)(评分范围:0 [无缺陷]至6 [死亡])在6、24个月时的发生率和并发症发生率。
结果 包括来自27个参与中风中心的73名儿童。中位年龄为11.3岁(四分位间距[IQR],7.0-15.0);男童37例(51%),女童36例(49%)。六十三名儿童(86%)接受了前循环闭塞治疗,十名患者(14%)接受了后循环闭塞治疗;16例患者(22%)同时接受了静脉溶栓治疗。神经学结果从入院时PedNIHSS的中位数14.0(IQR,9.2-20.0)改善到第7天的4.0(IQR,2.0-7.3),在6个月时的mRS得分中位数为1.0(IQR,0-1.6),而在6个月时为1.0(IQR,0-1.6)。 IQR,0-1.0)在24个月时。一名患者(1%)发生了介入后出血并发症,而四名患者(5%)发生了短暂性围手术期血管痉挛。
结论与相关性 这项研究的结果表明,儿童卒中的血栓切除术的安全性与成人随机临床试验中的安全性没有区别。大多数接受治疗的儿童的神经系统结局良好。这项研究可能会在缺乏高级证据的情况下支持临床医生在儿童卒中中实施标签外血栓切除术的实践。











































 京公网安备 11010802027423号
京公网安备 11010802027423号