Signal Transduction and Targeted Therapy ( IF 40.8 ) Pub Date : 2019-10-12 , DOI: 10.1038/s41392-019-0075-4 Mrinal K Ghosh 1 , Dipankar Chakraborty 1 , Sibani Sarkar 1 , Arijit Bhowmik 2 , Malini Basu 3
|
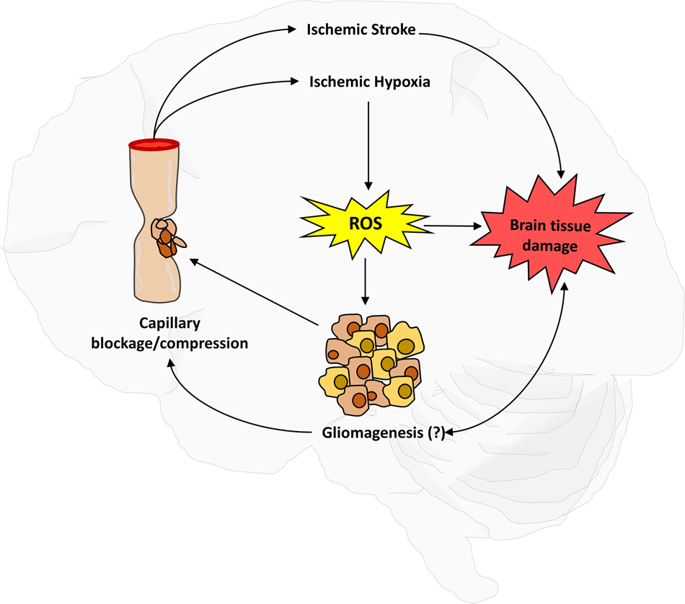
Glioma and cerebral ischemic stroke are two major events that lead to patient death worldwide. Although these conditions have different physiological incidences, ~10% of ischemic stroke patients develop cerebral cancer, especially glioma, in the postischemic stages. Additionally, the high proliferation, venous thrombosis and hypercoagulability of the glioma mass increase the significant risk of thromboembolism, including ischemic stroke. Surprisingly, these events share several common pathways, viz. hypoxia, cerebral inflammation, angiogenesis, etc., but the proper mechanism behind this co-occurrence has yet to be discovered. The hypercoagulability and presence of the D-dimer level in stroke are different in cancer patients than in the noncancerous population. Other factors such as atherosclerosis and coagulopathy involved in the pathogenesis of stroke are partially responsible for cancer, and the reverse is also partially true. Based on clinical and neurosurgical experience, the neuronal structures and functions in the brain and spine are observed to change after a progressive attack of ischemia that leads to hypoxia and atrophy. The major population of cancer cells cannot survive in an adverse ischemic environment that excludes cancer stem cells (CSCs). Cancer cells in stroke patients have already metastasized, but early-stage cancer patients also suffer stroke for multiple reasons. Therefore, stroke is an early manifestation of cancer. Stroke and cancer share many factors that result in an increased risk of stroke in cancer patients, and vice-versa. The intricate mechanisms for stroke with and without cancer are different. This review summarizes the current clinical reports, pathophysiology, probable causes of co-occurrence, prognoses, and treatment possibilities.
中文翻译:

脑缺血性卒中与神经胶质瘤之间的相互关系:近期报告的综合研究
神经胶质瘤和脑缺血性中风是导致全世界患者死亡的两个主要事件。尽管这些病症的生理发生率不同,但约有 10% 的缺血性中风患者在缺血后阶段发展为脑癌,尤其是神经胶质瘤。此外,神经胶质瘤块的高增殖、静脉血栓形成和高凝性增加了血栓栓塞(包括缺血性中风)的显着风险。令人惊讶的是,这些事件有几个共同的途径,即。缺氧、脑炎症、血管生成等,但这种同时发生背后的正确机制尚未被发现。癌症患者中风中的高凝状态和 D-二聚体水平的存在与非癌症人群不同。中风发病机制中涉及的其他因素,如动脉粥样硬化和凝血功能障碍,也是导致癌症的部分原因,反之亦然。根据临床和神经外科经验,观察到大脑和脊柱的神经元结构和功能在缺血进行性发作后发生变化,导致缺氧和萎缩。大多数癌细胞无法在排除癌症干细胞(CSC)的不利缺血环境中生存。中风患者体内的癌细胞已经转移,但早期癌症患者也会因为多种原因而遭受中风。因此,中风是癌症的早期表现。中风和癌症有许多共同因素,导致癌症患者中风风险增加,反之亦然。患有癌症和不患有癌症的中风的复杂机制是不同的。本综述总结了当前的临床报告、病理生理学、同时发生的可能原因、预后和治疗可能性。











































 京公网安备 11010802027423号
京公网安备 11010802027423号