Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Changes in End-of-Life Practices in European Intensive Care Units From 1999 to 2016
JAMA ( IF 63.1 ) Pub Date : 2019-11-05 , DOI: 10.1001/jama.2019.14608 Charles L Sprung 1 , Bara Ricou 2 , Christiane S Hartog 3 , Paulo Maia 4 , Spyros D Mentzelopoulos 5 , Manfred Weiss 6 , Phillip D Levin 7 , Laura Galarza 8 , Veronica de la Guardia 1 , Joerg C Schefold 9 , Mario Baras 10 , Gavin M Joynt 11 , Hans-Henrik Bülow 12 , Georgios Nakos 13 , Vladimir Cerny 14 , Stephan Marsch 15 , Armand R Girbes 16 , Catherine Ingels 17 , Orsolya Miskolci 18 , Didier Ledoux 19 , Sudakshina Mullick 20 , Maria G Bocci 21 , Jakob Gjedsted 22 , Belén Estébanez 23 , Joseph L Nates 24 , Olivier Lesieur 25 , Roshni Sreedharan 26 , Alberto M Giannini 27 , Lucía Cachafeiro Fuciños 23 , Christopher M Danbury 28 , Andrej Michalsen 29 , Ivo W Soliman 30 , Angel Estella 31 , Alexander Avidan 1
JAMA ( IF 63.1 ) Pub Date : 2019-11-05 , DOI: 10.1001/jama.2019.14608 Charles L Sprung 1 , Bara Ricou 2 , Christiane S Hartog 3 , Paulo Maia 4 , Spyros D Mentzelopoulos 5 , Manfred Weiss 6 , Phillip D Levin 7 , Laura Galarza 8 , Veronica de la Guardia 1 , Joerg C Schefold 9 , Mario Baras 10 , Gavin M Joynt 11 , Hans-Henrik Bülow 12 , Georgios Nakos 13 , Vladimir Cerny 14 , Stephan Marsch 15 , Armand R Girbes 16 , Catherine Ingels 17 , Orsolya Miskolci 18 , Didier Ledoux 19 , Sudakshina Mullick 20 , Maria G Bocci 21 , Jakob Gjedsted 22 , Belén Estébanez 23 , Joseph L Nates 24 , Olivier Lesieur 25 , Roshni Sreedharan 26 , Alberto M Giannini 27 , Lucía Cachafeiro Fuciños 23 , Christopher M Danbury 28 , Andrej Michalsen 29 , Ivo W Soliman 30 , Angel Estella 31 , Alexander Avidan 1
Affiliation
|
Importance
End-of-life decisions occur daily in intensive care units (ICUs) around the world, and these practices could change over time. Objective
To determine the changes in end-of-life practices in European ICUs after 16 years. Design, Setting, and Participants
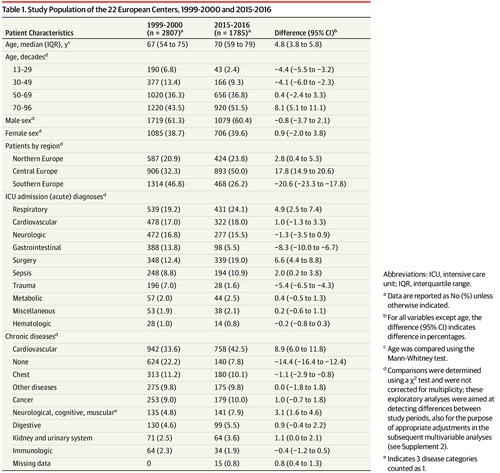
Ethicus-2 was a prospective observational study of 22 European ICUs previously included in the Ethicus-1 study (1999-2000). During a self-selected continuous 6-month period at each ICU, consecutive patients who died or had any limitation of life-sustaining therapy from September 2015 until October 2016 were included. Patients were followed up until death or until 2 months after the first treatment limitation decision. Exposures
Comparison between the 1999-2000 cohort vs 2015-2016 cohort. Main Outcomes and Measures
End-of-life outcomes were classified into 5 mutually exclusive categories (withholding of life-prolonging therapy, withdrawing of life-prolonging therapy, active shortening of the dying process, failed cardiopulmonary resuscitation [CPR], brain death). The primary outcome was whether patients received any treatment limitations (withholding or withdrawing of life-prolonging therapy or shortening of the dying process). Outcomes were determined by senior intensivists. Results
Of 13 625 patients admitted to participating ICUs during the 2015-2016 study period, 1785 (13.1%) died or had limitations of life-prolonging therapies and were included in the study. Compared with the patients included in the 1999-2000 cohort (n = 2807), the patients in 2015-2016 cohort were significantly older (median age, 70 years [interquartile range {IQR}, 59-79] vs 67 years [IQR, 54-75]; P < .001) and the proportion of female patients was similar (39.6% vs 38.7%; P = .58). Significantly more treatment limitations occurred in the 2015-2016 cohort compared with the 1999-2000 cohort (1601 [89.7%] vs 1918 [68.3%]; difference, 21.4% [95% CI, 19.2% to 23.6%]; P < .001), with more withholding of life-prolonging therapy (892 [50.0%] vs 1143 [40.7%]; difference, 9.3% [95% CI, 6.4% to 12.3%]; P < .001), more withdrawing of life-prolonging therapy (692 [38.8%] vs 695 [24.8%]; difference, 14.0% [95% CI, 11.2% to 16.8%]; P < .001), less failed CPR (110 [6.2%] vs 628 [22.4%]; difference, -16.2% [95% CI, -18.1% to -14.3%]; P < .001), less brain death (74 [4.1%] vs 261 [9.3%]; difference, -5.2% [95% CI, -6.6% to -3.8%]; P < .001) and less active shortening of the dying process (17 [1.0%] vs 80 [2.9%]; difference, -1.9% [95% CI, -2.7% to -1.1%]; P < .001). Conclusions and Relevance
Among patients who had treatment limitations or died in 22 European ICUs in 2015-2016, compared with data reported from the same ICUs in 1999-2000, limitations in life-prolonging therapies occurred significantly more frequently and death without limitations in life-prolonging therapies occurred significantly less frequently. These findings suggest a shift in end-of-life practices in European ICUs, but the study is limited in that it excluded patients who survived ICU hospitalization without treatment limitations.
中文翻译:

1999 年至 2016 年欧洲重症监护病房临终实践的变化
重要性 世界各地的重症监护病房 (ICU) 每天都会做出临终决定,这些做法可能会随着时间而改变。目的 确定 16 年后欧洲 ICU 临终实践的变化。设计、设置和参与者 Ethicus-2 是一项前瞻性观察研究,对 22 个欧洲 ICU 先前纳入 Ethicus-1 研究(1999-2000)。在每个 ICU 的自选连续 6 个月期间,包括 2015 年 9 月至 2016 年 10 月期间死亡或生命维持治疗有任何限制的连续患者。对患者进行随访直至死亡或第一次治疗限制决定后 2 个月。1999-2000 年队列与 2015-2016 年队列之间的暴露比较。主要结果和措施 临终结果分为 5 个相互排斥的类别(停止延长生命治疗、停止延长生命治疗、主动缩短死亡过程、心肺复苏术 [CPR] 失败、脑死亡)。主要结果是患者是否接受任何治疗限制(拒绝或停止延长生命的治疗或缩短死亡过程)。结果由高级重症监护医师确定。结果 2015-2016 年研究期间,13625 名入住 ICU 的患者中,1785 名(13.1%)死亡或延长生命的治疗受到限制,并被纳入研究。与 1999-2000 年队列中的患者(n = 2807)相比,2015-2016 年队列中的患者年龄明显更大(中位年龄,70 岁 [四分位距 {IQR},59-79] 与 67 岁 [IQR,54-75];P < .001)和女性患者的比例相似(39.6% vs 38.7%;P = .58)。与 1999-2000 年队列相比,2015-2016 年队列出现了更多的治疗限制(1601 [89.7%] vs 1918 [68.3%];差异为 21.4% [95% CI,19.2% 至 23.6%];P < . 001),延长生命的治疗停止更多(892 [50.0%] vs 1143 [40.7%];差异,9.3% [95% CI,6.4% 至 12.3%];P < .001),更多的生命退出- 延长治疗时间(692 [38.8%] vs 695 [24.8%];差异,14.0% [95% CI,11.2% 至 16.8%];P < .001),CPR 失败率更低(110 [6.2%] vs 628 [ 22.4%];差异,-16.2% [95% CI,-18.1% 至 -14.3%];P < .001),更少的脑死亡(74 [4.1%] vs 261 [9.3%];差异,-5.2% [95% CI,-6.6% 至 -3.8%];P < . 001)和较少主动缩短死亡过程(17 [1.0%] vs 80 [2.9%];差异,-1.9% [95% CI,-2.7% 至 -1.1%];P < .001)。结论和相关性 在 2015-2016 年在 22 个欧洲 ICU 中出现治疗限制或死亡的患者中,与 1999-2000 年同一 ICU 报告的数据相比,延长生命治疗的限制发生率明显更高,死亡无生命限制延长治疗的发生频率明显降低。这些发现表明欧洲 ICU 的临终实践发生了转变,但该研究的局限性在于它排除了在没有治疗限制的情况下在 ICU 住院中幸存下来的患者。结论和相关性 在 2015-2016 年在 22 个欧洲 ICU 中治疗受限或死亡的患者中,与 1999-2000 年同一 ICU 报告的数据相比,延长生命治疗受限的发生率明显更高,死亡无生命受限延长治疗的发生频率明显降低。这些发现表明欧洲 ICU 的临终实践发生了转变,但该研究的局限性在于它排除了在没有治疗限制的情况下在 ICU 住院中幸存下来的患者。结论和相关性 在 2015-2016 年在 22 个欧洲 ICU 中治疗受限或死亡的患者中,与 1999-2000 年同一 ICU 报告的数据相比,延长生命治疗受限的发生率明显更高,死亡无生命受限延长治疗的发生频率明显降低。这些发现表明欧洲 ICU 的临终实践发生了转变,但该研究的局限性在于它排除了在没有治疗限制的情况下在 ICU 住院中幸存下来的患者。
更新日期:2019-11-05
中文翻译:

1999 年至 2016 年欧洲重症监护病房临终实践的变化
重要性 世界各地的重症监护病房 (ICU) 每天都会做出临终决定,这些做法可能会随着时间而改变。目的 确定 16 年后欧洲 ICU 临终实践的变化。设计、设置和参与者 Ethicus-2 是一项前瞻性观察研究,对 22 个欧洲 ICU 先前纳入 Ethicus-1 研究(1999-2000)。在每个 ICU 的自选连续 6 个月期间,包括 2015 年 9 月至 2016 年 10 月期间死亡或生命维持治疗有任何限制的连续患者。对患者进行随访直至死亡或第一次治疗限制决定后 2 个月。1999-2000 年队列与 2015-2016 年队列之间的暴露比较。主要结果和措施 临终结果分为 5 个相互排斥的类别(停止延长生命治疗、停止延长生命治疗、主动缩短死亡过程、心肺复苏术 [CPR] 失败、脑死亡)。主要结果是患者是否接受任何治疗限制(拒绝或停止延长生命的治疗或缩短死亡过程)。结果由高级重症监护医师确定。结果 2015-2016 年研究期间,13625 名入住 ICU 的患者中,1785 名(13.1%)死亡或延长生命的治疗受到限制,并被纳入研究。与 1999-2000 年队列中的患者(n = 2807)相比,2015-2016 年队列中的患者年龄明显更大(中位年龄,70 岁 [四分位距 {IQR},59-79] 与 67 岁 [IQR,54-75];P < .001)和女性患者的比例相似(39.6% vs 38.7%;P = .58)。与 1999-2000 年队列相比,2015-2016 年队列出现了更多的治疗限制(1601 [89.7%] vs 1918 [68.3%];差异为 21.4% [95% CI,19.2% 至 23.6%];P < . 001),延长生命的治疗停止更多(892 [50.0%] vs 1143 [40.7%];差异,9.3% [95% CI,6.4% 至 12.3%];P < .001),更多的生命退出- 延长治疗时间(692 [38.8%] vs 695 [24.8%];差异,14.0% [95% CI,11.2% 至 16.8%];P < .001),CPR 失败率更低(110 [6.2%] vs 628 [ 22.4%];差异,-16.2% [95% CI,-18.1% 至 -14.3%];P < .001),更少的脑死亡(74 [4.1%] vs 261 [9.3%];差异,-5.2% [95% CI,-6.6% 至 -3.8%];P < . 001)和较少主动缩短死亡过程(17 [1.0%] vs 80 [2.9%];差异,-1.9% [95% CI,-2.7% 至 -1.1%];P < .001)。结论和相关性 在 2015-2016 年在 22 个欧洲 ICU 中出现治疗限制或死亡的患者中,与 1999-2000 年同一 ICU 报告的数据相比,延长生命治疗的限制发生率明显更高,死亡无生命限制延长治疗的发生频率明显降低。这些发现表明欧洲 ICU 的临终实践发生了转变,但该研究的局限性在于它排除了在没有治疗限制的情况下在 ICU 住院中幸存下来的患者。结论和相关性 在 2015-2016 年在 22 个欧洲 ICU 中治疗受限或死亡的患者中,与 1999-2000 年同一 ICU 报告的数据相比,延长生命治疗受限的发生率明显更高,死亡无生命受限延长治疗的发生频率明显降低。这些发现表明欧洲 ICU 的临终实践发生了转变,但该研究的局限性在于它排除了在没有治疗限制的情况下在 ICU 住院中幸存下来的患者。结论和相关性 在 2015-2016 年在 22 个欧洲 ICU 中治疗受限或死亡的患者中,与 1999-2000 年同一 ICU 报告的数据相比,延长生命治疗受限的发生率明显更高,死亡无生命受限延长治疗的发生频率明显降低。这些发现表明欧洲 ICU 的临终实践发生了转变,但该研究的局限性在于它排除了在没有治疗限制的情况下在 ICU 住院中幸存下来的患者。









































 京公网安备 11010802027423号
京公网安备 11010802027423号