Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of General Anesthesia vs Procedural Sedation With Functional Outcome Among Patients With Acute Ischemic Stroke Undergoing Thrombectomy
JAMA ( IF 63.1 ) Pub Date : 2019-10-01 , DOI: 10.1001/jama.2019.11455 Silvia Schönenberger 1 , Pia Löwhagen Hendén 2 , Claus Z Simonsen 3 , Lorenz Uhlmann 4 , Christina Klose 4 , Johannes A R Pfaff 5 , Albert J Yoo 6 , Leif H Sørensen 7 , Peter A Ringleb 1 , Wolfgang Wick 1, 8 , Meinhard Kieser 4 , Markus A Möhlenbruch 5 , Mads Rasmussen 9 , Alexandros Rentzos 10 , Julian Bösel 11
JAMA ( IF 63.1 ) Pub Date : 2019-10-01 , DOI: 10.1001/jama.2019.11455 Silvia Schönenberger 1 , Pia Löwhagen Hendén 2 , Claus Z Simonsen 3 , Lorenz Uhlmann 4 , Christina Klose 4 , Johannes A R Pfaff 5 , Albert J Yoo 6 , Leif H Sørensen 7 , Peter A Ringleb 1 , Wolfgang Wick 1, 8 , Meinhard Kieser 4 , Markus A Möhlenbruch 5 , Mads Rasmussen 9 , Alexandros Rentzos 10 , Julian Bösel 11
Affiliation
|
Importance
General anesthesia during thrombectomy for acute ischemic stroke has been associated with poor neurological outcome in nonrandomized studies. Three single-center randomized trials reported no significantly different or improved outcomes for patients who received general anesthesia compared with procedural sedation. Objective
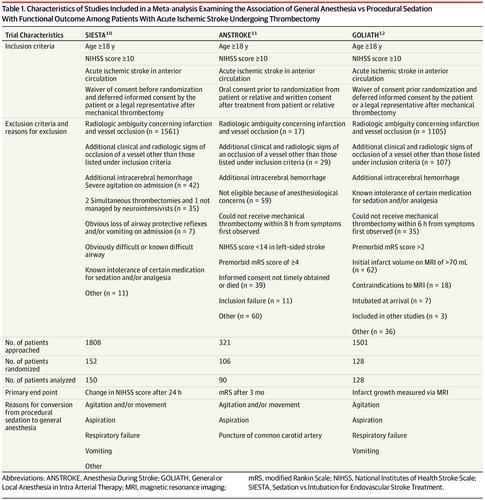
To detect differences in functional outcome at 3 months between patients who received general anesthesia vs procedural sedation during thrombectomy for anterior circulation acute ischemic stroke. Data Source
MEDLINE search for English-language articles published from January 1, 1980, to July 31, 2019. Study Selection
Randomized clinical trials of adults with a National Institutes of Health Stroke Scale score of at least 10 and anterior circulation acute ischemic stroke assigned to receive general anesthesia or procedural sedation during thrombectomy. Data Extraction and Synthesis
Individual patient data were obtained from 3 single-center, randomized, parallel-group, open-label treatment trials with blinded end point evaluation that met inclusion criteria and were analyzed using fixed-effects meta-analysis. Main Outcomes and Measures
Degree of disability, measured via the modified Rankin Scale (mRS) score (range 0-6; lower scores indicate less disability), analyzed with the common odds ratio (cOR) to detect the ordinal shift in the distribution of disability over the range of mRS scores. Results
A total of 368 patients (mean [SD] age, 71.5 [12.9] years; 163 [44.3%] women; median [interquartile range] National Institutes of Health Stroke Scale score, 17 [14-21]) were included in the analysis, including 183 (49.7%) who received general anesthesia and 185 (50.3%) who received procedural sedation. The mean 3-month mRS score was 2.8 (95% CI, 2.5-3.1) in the general anesthesia group vs 3.2 (95% CI, 3.0-3.5) in the procedural sedation group (difference, 0.43 [95% CI, 0.03-0.83]; cOR, 1.58 [95% CI, 1.09-2.29]; P = .02). Among prespecified adverse events, only hypotension (decline in systolic blood pressure of more than 20% from baseline) (80.8% vs 53.1%; OR, 4.26 [95% CI, 2.55-7.09]; P < .001) and blood pressure variability (systolic blood pressure >180 mm Hg or <120 mm Hg) (79.7 vs 62.3%; OR, 2.42 [95% CI, 1.49-3.93]; P < .001) were significantly more common in the general anesthesia group. Conclusions and Relevance
Among patients with acute ischemic stroke involving the anterior circulation undergoing thrombectomy, the use of protocol-based general anesthesia, compared with procedural sedation, was significantly associated with less disability at 3 months. These findings should be interpreted tentatively, given that the individual trials examined were single-center trials and disability was the primary outcome in only 1 trial.
中文翻译:

在接受血栓切除术的急性缺血性卒中患者中,全身麻醉与程序性镇静与功能结果的关系
重要性 在非随机研究中,急性缺血性卒中取栓期间的全身麻醉与不良的神经系统预后相关。三项单中心随机试验报告,与程序性镇静相比,接受全身麻醉的患者的结局没有显着差异或改善。目的 检测前循环急性缺血性卒中取栓术中全身麻醉与程序性镇静患者 3 个月功能结局的差异。数据源 MEDLINE 搜索 1980 年 1 月 1 日至 2019 年 7 月 31 日发表的英文文章。研究选择美国国立卫生研究院卒中量表评分至少为 10 分且前循环急性缺血性卒中被分配接受全身麻醉或血栓切除术过程镇静的成人的随机临床试验。数据提取和综合 个体患者数据来自 3 个单中心、随机、平行组、开放标签治疗试验,这些试验具有符合纳入标准的盲法终点评估,并使用固定效应荟萃分析进行分析。主要结果和措施 残疾程度,通过改良的 Rankin 量表 (mRS) 评分(范围 0-6;分数越低表示残疾越少),用共同优势比 (cOR) 分析以检测残疾分布的序数变化在 mRS 评分范围内。结果 共有 368 名患者(平均 [SD] 年龄,71.5 [12. 9]年;163 [44.3%] 名女性;中位数 [四分位距] 美国国立卫生研究院卒中量表评分,17 [14-21]) 被纳入分析,其中 183 人 (49.7%) 接受了全身麻醉,185 人 (50.3%) 接受了程序镇静。全身麻醉组平均 3 个月 mRS 评分为 2.8 (95% CI, 2.5-3.1),而程序镇静组为 3.2 (95% CI, 3.0-3.5)(差异,0.43 [95% CI, 0.03- 0.83];cOR,1.58 [95% CI,1.09-2.29];P = .02)。在预先设定的不良事件中,只有低血压(收缩压比基线下降超过 20%)(80.8% vs 53.1%;OR,4.26 [95% CI,2.55-7.09];P < .001)和血压变异性(收缩压 >180 mm Hg 或 <120 mm Hg)(79.7 对 62.3%;OR,2.42 [95% CI,1.49-3.93];P < . 001)在全身麻醉组中更为常见。结论和相关性 在接受血栓切除术的前循环急性缺血性卒中患者中,与程序性镇静相比,使用基于方案的全身麻醉与 3 个月时的残疾减少显着相关。鉴于所检查的个别试验是单中心试验,并且残疾是仅 1 项试验的主要结果,这些发现应作初步解释。
更新日期:2019-10-01
中文翻译:

在接受血栓切除术的急性缺血性卒中患者中,全身麻醉与程序性镇静与功能结果的关系
重要性 在非随机研究中,急性缺血性卒中取栓期间的全身麻醉与不良的神经系统预后相关。三项单中心随机试验报告,与程序性镇静相比,接受全身麻醉的患者的结局没有显着差异或改善。目的 检测前循环急性缺血性卒中取栓术中全身麻醉与程序性镇静患者 3 个月功能结局的差异。数据源 MEDLINE 搜索 1980 年 1 月 1 日至 2019 年 7 月 31 日发表的英文文章。研究选择美国国立卫生研究院卒中量表评分至少为 10 分且前循环急性缺血性卒中被分配接受全身麻醉或血栓切除术过程镇静的成人的随机临床试验。数据提取和综合 个体患者数据来自 3 个单中心、随机、平行组、开放标签治疗试验,这些试验具有符合纳入标准的盲法终点评估,并使用固定效应荟萃分析进行分析。主要结果和措施 残疾程度,通过改良的 Rankin 量表 (mRS) 评分(范围 0-6;分数越低表示残疾越少),用共同优势比 (cOR) 分析以检测残疾分布的序数变化在 mRS 评分范围内。结果 共有 368 名患者(平均 [SD] 年龄,71.5 [12. 9]年;163 [44.3%] 名女性;中位数 [四分位距] 美国国立卫生研究院卒中量表评分,17 [14-21]) 被纳入分析,其中 183 人 (49.7%) 接受了全身麻醉,185 人 (50.3%) 接受了程序镇静。全身麻醉组平均 3 个月 mRS 评分为 2.8 (95% CI, 2.5-3.1),而程序镇静组为 3.2 (95% CI, 3.0-3.5)(差异,0.43 [95% CI, 0.03- 0.83];cOR,1.58 [95% CI,1.09-2.29];P = .02)。在预先设定的不良事件中,只有低血压(收缩压比基线下降超过 20%)(80.8% vs 53.1%;OR,4.26 [95% CI,2.55-7.09];P < .001)和血压变异性(收缩压 >180 mm Hg 或 <120 mm Hg)(79.7 对 62.3%;OR,2.42 [95% CI,1.49-3.93];P < . 001)在全身麻醉组中更为常见。结论和相关性 在接受血栓切除术的前循环急性缺血性卒中患者中,与程序性镇静相比,使用基于方案的全身麻醉与 3 个月时的残疾减少显着相关。鉴于所检查的个别试验是单中心试验,并且残疾是仅 1 项试验的主要结果,这些发现应作初步解释。











































 京公网安备 11010802027423号
京公网安备 11010802027423号