当前位置:
X-MOL 学术
›
JAMA Oncol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Factors Associated With Successful Discontinuation of Immune Suppression After Allogeneic Hematopoietic Cell Transplantation.
JAMA Oncology ( IF 22.5 ) Pub Date : 2019-09-26 , DOI: 10.1001/jamaoncol.2019.2974 Joseph Pidala 1 , Michael Martens 2 , Claudio Anasetti 1 , Jeanette Carreras 3 , Mary Horowitz 4 , Stephanie J Lee 5 , Joseph Antin 6 , Corey Cutler 6 , Brent Logan 7
JAMA Oncology ( IF 22.5 ) Pub Date : 2019-09-26 , DOI: 10.1001/jamaoncol.2019.2974 Joseph Pidala 1 , Michael Martens 2 , Claudio Anasetti 1 , Jeanette Carreras 3 , Mary Horowitz 4 , Stephanie J Lee 5 , Joseph Antin 6 , Corey Cutler 6 , Brent Logan 7
Affiliation
|
Importance
Immune suppression discontinuation is routinely attempted after allogeneic hematopoietic cell transplantation (HCT) and under current practices may lead to graft-vs-host disease (GVHD)-associated morbidity and death. However, the likelihood and predictive factors associated with successful immune suppression discontinuation after HCT are poorly understood.
Objectives
To examine factors associated with successful immune suppression discontinuation and risk for immune suppression discontinuation failure under conventional HCT approaches and develop a practical tool to estimate successful immune suppression discontinuation likelihood at the clinical point of care.
Design, Setting, and Participants
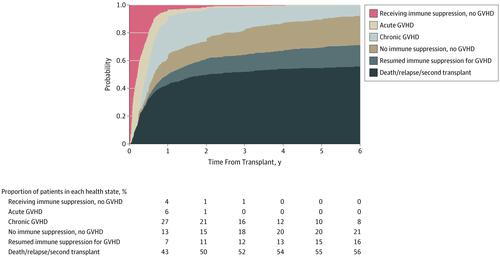
Using long-term follow-up data from 2 national Blood and Marrow Transplant Clinical Trial Network studies (N = 827), a multistate model was developed to investigate the probability and variables associated with immune suppression discontinuation success. The study began in July 2015, and analyses were completed in August 2019.
Main Outcomes and Measures
Immune suppression discontinuation and immune suppression discontinuation failure.
Results
Of the 827 patients included in the analysis, 456 were men (55.1%). Median age at transplant was 44 (range, <1-67) years. With median follow-up of 72 (range, 11-124) months, 20.0% of the patients were alive and not receiving immune suppression at 5 years. Older recipient age (adjusted odds ratio [aOR] of >50 vs <30 years, 0.27, 99% CI, 0.14-0.50; P < .001), mismatched unrelated donor (aOR, mismatched unrelated vs matched related, 0.37; 99% CI, 0.14-0.97; P = .008), peripheral blood graft (aOR of peripheral blood graft vs bone marrow, 0.46; 99% CI, 0.26-0.82; P < .001), and advanced stage disease (aOR of advanced vs early disease, 0.45; 99% CI, 0.23-0.86, P = 0.002), were significantly associated with decreased odds of immune suppression discontinuation. Failed attempts at immune suppression discontinuation (127 patients [37.1% of total immune suppression discontinuation events]) resulting in GVHD were significantly associated with use of peripheral blood stem cells (HR, 2.62; 99% CI, 1.30-5.29; P < .001), prior GVHD, and earlier immune suppression discontinuation attempts. Earlier immune suppression discontinuation was not associated with protection from cancer relapse after HCT (adjusted hazard ratio for discontinuation vs not, 1.95; 99% CI, 0.88-4.31; P = .03).Dynamic prediction models were developed to provide future immune suppression discontinuation probability according to individual patient characteristics.
Conclusions and Relevance
Successful immune suppression discontinuation is uncommon in the setting of peripheral blood stem cell grafts. The data suggest earlier attempts at ISD conferred no long-term benefit, given frequent ISD failure, limited subsequent success after initial failed ISD attempt, and no evidence of relapse reduction. Using a risk model-based clinical application, physicians may be able to identify individual patients' probability of successful immune suppression discontinuation.
中文翻译:

异基因造血细胞移植后成功终止免疫抑制的相关因素。
重要性 同种异体造血细胞移植 (HCT) 后常规尝试停止免疫抑制,根据目前的做法可能导致移植物抗宿主病 (GVHD) 相关的发病率和死亡。然而,人们对 HCT 后成功终止免疫抑制相关的可能性和预测因素知之甚少。目的 研究在传统 HCT 方法下与成功终止免疫抑制相关的因素和免疫抑制终止失败的风险,并开发一种实用工具来估计临床护理点成功的免疫抑制终止可能性。设计、设置和参与者使用来自 2 个国家血液和骨髓移植临床试验网络研究 (N = 827) 的长期随访数据,开发了一个多状态模型来研究与免疫抑制终止成功相关的概率和变量。该研究于2015年7月开始,分析于2019年8月完成。主要结果和措施免疫抑制停药和免疫抑制停药失败。结果 在纳入分析的 827 名患者中,456 名是男性(55.1%)。移植时的中位年龄为 44(范围,<1-67)岁。中位随访时间为 72(范围,11-124)个月,20.0% 的患者在 5 年时存活且未接受免疫抑制。受者年龄较大(调整优势比 [aOR] >50 vs <30 岁,0.27,99% CI,0.14-0.50;P < .001),不匹配的无关供者(aOR,不匹配的无关与匹配的相关,0.37;99% CI,0.14-0.97;P = .008),外周血移植物(外周血移植物与骨髓的 aOR,0.46;99% CI,0.26-0.82;P < .001)和晚期疾病(晚期与早期疾病的 aOR,0.45;99% CI,0.23-0.86 , P = 0.002),与免疫抑制终止几率降低显着相关。导致 GVHD 的免疫抑制终止尝试失败(127 名患者 [37.1% 的总免疫抑制终止事件])与外周血干细胞的使用显着相关(HR,2.62;99% CI,1.30-5.29;P < .001 )、先前的 GVHD 和早期的免疫抑制终止尝试。早期免疫抑制终止与 HCT 后癌症复发的保护无关(调整后的终止与不终止的风险比,1.95;99% CI,0.88-4.31;P = .03)。开发了动态预测模型以根据个体患者特征提供未来的免疫抑制终止概率。结论和相关性 在外周血干细胞移植的情况下,成功终止免疫抑制并不常见。数据表明,早期的 ISD 尝试并没有带来长期的益处,因为 ISD 经常失败,在最初的 ISD 尝试失败后后续成功有限,并且没有减少复发的证据。使用基于风险模型的临床应用,医生可能能够确定个体患者成功停用免疫抑制的概率。结论和相关性 在外周血干细胞移植的情况下,成功终止免疫抑制并不常见。数据表明,早期的 ISD 尝试并没有带来长期的益处,因为 ISD 经常失败,在最初的 ISD 尝试失败后后续成功有限,并且没有减少复发的证据。使用基于风险模型的临床应用,医生可能能够确定个体患者成功停用免疫抑制的概率。结论和相关性 在外周血干细胞移植的情况下,成功终止免疫抑制并不常见。数据表明,早期的 ISD 尝试并没有带来长期的益处,因为 ISD 经常失败,在最初的 ISD 尝试失败后后续成功有限,并且没有减少复发的证据。使用基于风险模型的临床应用,医生可能能够确定个体患者成功停用免疫抑制的概率。
更新日期:2020-01-09
中文翻译:

异基因造血细胞移植后成功终止免疫抑制的相关因素。
重要性 同种异体造血细胞移植 (HCT) 后常规尝试停止免疫抑制,根据目前的做法可能导致移植物抗宿主病 (GVHD) 相关的发病率和死亡。然而,人们对 HCT 后成功终止免疫抑制相关的可能性和预测因素知之甚少。目的 研究在传统 HCT 方法下与成功终止免疫抑制相关的因素和免疫抑制终止失败的风险,并开发一种实用工具来估计临床护理点成功的免疫抑制终止可能性。设计、设置和参与者使用来自 2 个国家血液和骨髓移植临床试验网络研究 (N = 827) 的长期随访数据,开发了一个多状态模型来研究与免疫抑制终止成功相关的概率和变量。该研究于2015年7月开始,分析于2019年8月完成。主要结果和措施免疫抑制停药和免疫抑制停药失败。结果 在纳入分析的 827 名患者中,456 名是男性(55.1%)。移植时的中位年龄为 44(范围,<1-67)岁。中位随访时间为 72(范围,11-124)个月,20.0% 的患者在 5 年时存活且未接受免疫抑制。受者年龄较大(调整优势比 [aOR] >50 vs <30 岁,0.27,99% CI,0.14-0.50;P < .001),不匹配的无关供者(aOR,不匹配的无关与匹配的相关,0.37;99% CI,0.14-0.97;P = .008),外周血移植物(外周血移植物与骨髓的 aOR,0.46;99% CI,0.26-0.82;P < .001)和晚期疾病(晚期与早期疾病的 aOR,0.45;99% CI,0.23-0.86 , P = 0.002),与免疫抑制终止几率降低显着相关。导致 GVHD 的免疫抑制终止尝试失败(127 名患者 [37.1% 的总免疫抑制终止事件])与外周血干细胞的使用显着相关(HR,2.62;99% CI,1.30-5.29;P < .001 )、先前的 GVHD 和早期的免疫抑制终止尝试。早期免疫抑制终止与 HCT 后癌症复发的保护无关(调整后的终止与不终止的风险比,1.95;99% CI,0.88-4.31;P = .03)。开发了动态预测模型以根据个体患者特征提供未来的免疫抑制终止概率。结论和相关性 在外周血干细胞移植的情况下,成功终止免疫抑制并不常见。数据表明,早期的 ISD 尝试并没有带来长期的益处,因为 ISD 经常失败,在最初的 ISD 尝试失败后后续成功有限,并且没有减少复发的证据。使用基于风险模型的临床应用,医生可能能够确定个体患者成功停用免疫抑制的概率。结论和相关性 在外周血干细胞移植的情况下,成功终止免疫抑制并不常见。数据表明,早期的 ISD 尝试并没有带来长期的益处,因为 ISD 经常失败,在最初的 ISD 尝试失败后后续成功有限,并且没有减少复发的证据。使用基于风险模型的临床应用,医生可能能够确定个体患者成功停用免疫抑制的概率。结论和相关性 在外周血干细胞移植的情况下,成功终止免疫抑制并不常见。数据表明,早期的 ISD 尝试并没有带来长期的益处,因为 ISD 经常失败,在最初的 ISD 尝试失败后后续成功有限,并且没有减少复发的证据。使用基于风险模型的临床应用,医生可能能够确定个体患者成功停用免疫抑制的概率。











































 京公网安备 11010802027423号
京公网安备 11010802027423号