JAMA Psychiatry ( IF 25.8 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamapsychiatry.2019.2741 David J R Morgan 1, 2 , Kwok M Ho 1, 3 , Cameron Platell 4, 5
|
Importance Obesity is associated with an increased prevalence of psychiatric disorders. The association of bariatric surgery with mental health outcomes is poorly understood.
Objective To investigate the association of bariatric surgery with the incidence of outpatient, emergency department (ED), and inpatient mental health service use.
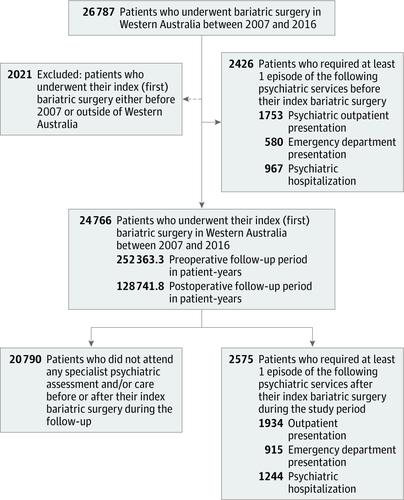
Design, Setting, and Participants This statewide, mirror-image, longitudinal cohort study used data from Western Australian Department of Health Data Linkage Branch records from all patients undergoing index (ie, first) bariatric surgery in Western Australia over a 10-year period (January 2007-December 2016), with mean (SD) follow-up periods of 10.2 (2.9) years before and 5.2 (2.9) years after index bariatric surgery. The data analysis was performed between November 2018 and March 2019.
Exposures Index bariatric surgery.
Main Outcomes and Measures The incidence and predictors for mental health presentations, deliberate self-harm, and suicide in association with the timing of bariatric surgery.
Results A total of 24 766 patients underwent index bariatric surgery; of these, the mean (SD) age was 42.5 (11.7) years and 19 144 (77.3%) were women. Use of at least 1 mental health service occurred in 3976 patients (16.1%), with 1401 patients (35.2%) presenting only before surgery, 1025 (25.8%) presenting before and after surgery, and 1550 patients (39.0%) presenting only after surgery. There was an increase in psychiatric illness presentations after bariatric surgery (outpatient clinic attendance: incidence rate ratio [IRR], 2.3; 95% CI, 2.3-2.4; ED attendance: IRR, 3.0; 95% CI, 2.8-3.2; psychiatric hospitalization: IRR, 3.0; 95% CI, 2.8-3.1). There was also a 5-fold increase in deliberate self-harm presentations to an ED after surgery (IRR, 4.7; 95% CI, 3.8-5.7), with 25 of 261 postoperatives deaths (9.6%) due to suicide. Complications after bariatric surgery requiring further surgical intervention and a history of mental health service provision before surgery were the most important associations with subsequent mental health presentations after surgery. Deliberate self-harm and mental and behavioral disorders due to psychoactive substance use before bariatric surgery were the main associations with subsequent deliberate self-harm or suicide after surgery.
Conclusions and Relevance We observed an increase in mental health service presentations after bariatric surgery, particularly among those who had prior psychiatric illnesses or developed surgical complications requiring further surgery. These findings caution the hypothesis that weight reduction by bariatric surgery will improve mental health in patients with obesity.
中文翻译:

减肥手术后心理健康服务使用的发生率和决定因素
重要性 肥胖与精神疾病患病率增加有关。人们对减肥手术与心理健康结果的关系知之甚少。
目的 调查减肥手术与门诊、急诊室 (ED) 和住院患者心理健康服务使用率的关系。
设计、设置和参与者 这项全州范围的镜像纵向队列研究使用了西澳大利亚州卫生部数据链接部门记录的数据,这些记录来自 10 年来在西澳大利亚州接受指数(即首次)减肥手术的所有患者( 2007 年 1 月至 2016 年 12 月),首次减肥手术前平均(SD)随访时间为 10.2(2.9)年,术后平均随访时间为 5.2(2.9)年。数据分析于2018年11月至2019年3月期间进行。
暴露 指数减肥手术。
主要结果和措施与 减肥手术时间相关的心理健康表现、故意自残和自杀的发生率和预测因素。
结果 共有24 766名患者接受了首次减肥手术;其中,平均 (SD) 年龄为 42.5 (11.7) 岁,其中 19 144 名 (77.3%) 为女性。3976 名患者 (16.1%) 至少使用过 1 次心理健康服务,其中 1401 名患者 (35.2%) 仅在手术前就诊,1025 名患者 (25.8%) 在手术前后就诊,1550 名患者 (39.0%) 仅在手术后就诊外科手术。减肥手术后精神疾病的发病率有所增加(门诊就诊:发病率比 [IRR],2.3;95% CI,2.3-2.4;急诊就诊:IRR,3.0;95% CI,2.8-3.2;精神病住院治疗:IRR,3.0;95% CI,2.8-3.1)。手术后向急诊科就诊的故意自残行为也增加了 5 倍(IRR,4.7;95% CI,3.8-5.7),261 例术后死亡中有 25 例(9.6%)死于自杀。减肥手术后需要进一步手术干预的并发症和术前提供心理健康服务的历史是与术后随后心理健康表现最重要的关联。减肥手术前因使用精神活性物质而导致的故意自残以及精神和行为障碍是与术后故意自残或自杀的主要关联。
结论和相关性 我们观察到减肥手术后心理健康服务的数量有所增加,特别是那些既往患有精神疾病或出现需要进一步手术的手术并发症的患者。这些发现提醒人们,通过减肥手术减轻体重将改善肥胖患者的心理健康。



























 京公网安备 11010802027423号
京公网安备 11010802027423号