JAMA Neurology ( IF 20.4 ) Pub Date : 2020-01-01 , DOI: 10.1001/jamaneurol.2019.2995 Albert R Moore 1 , Paul M Wieczorek 2 , Jose C A Carvalho 3
|
Importance Women giving birth have high rates of dural puncture secondary to neuraxial anesthesia and are at high risk for a resulting headache. It appears to be unknown whether there is a significant association between post–dural puncture headache and subsequent intracranial subdural hematoma.
Objective To determine the association of post–dural puncture headache with postpartum intracranial subdural hematoma.
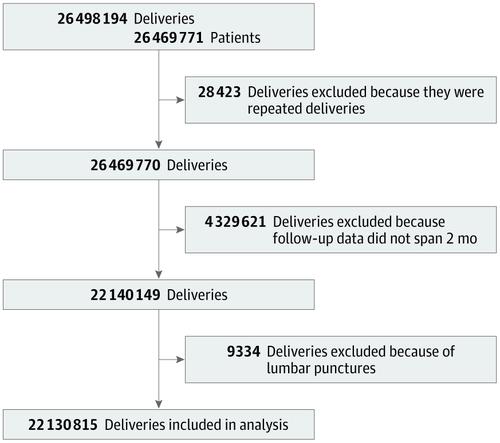
Design, Setting, and Participants This cohort study of patients used hospital discharges recorded in the US Agency for Healthcare Research and Quality National Readmission Database for women who experienced childbirth from January 2010 to December 2016. Patients were included if they had been admitted for childbirth, had 2 months of follow-up data, and did not receive a diagnostic lumbar puncture. Only the first delivery for a calendar year was studied. Data were analyzed from January 2018 to June 2019.
Exposures Women with post–dural puncture headache associated with neuraxial anesthesia in the 2-month postpartum period were identified using International Classification of Disease (Ninth Edition and Tenth Edition) codes and were compared with those without post–dural puncture headaches.
Main Outcome and Measures The primary outcome was intracranial subdural hematoma in the 2-month postpartum period. Secondary outcomes included in-hospital mortality and occurrence of neurosurgery.
Results A total of 26 469 771 patients with 26 498 194 deliveries were included. Exclusion of repeated deliveries (n = 28 423), deliveries without 2 months of follow-up data (n = 4 329 621), and deliveries with diagnostic lumbar puncture (n = 9334) resulted in a final cohort of 22 130 815 patients and deliveries. For the cohort, the mean (SD) age was 28.1 (6.0) years, and there were 68 374 post–dural puncture headaches, for an overall rate of 309 (95% CI, 302-316) per 100 000. There were 342 cases of subdural hematoma identified, indicating a rate of 1.5 (95% CI, 1.3-1.8) per 100 000 women. Of these, 100 cases were in women with post–dural puncture headache, indicating a rate of 147 (95% CI, 111-194) hematoma cases per 100 000 deliveries in this subgroup. Post–dural puncture headache had an unadjusted absolute risk increase of 145 (95% CI, 117-174) subdural hematoma cases per 100 000 deliveries. After adjusting for confounders, post–dural puncture headache had an odds ratio for subdural hematoma of 199 (95% CI, 126-317; P < .001) and an adjusted absolute risk increase of 130 (95% CI, 90-169; P < .001) per 100 000 deliveries.
Conclusions and Relevance The presence of presumed post–dural puncture headache after neuraxial anesthesia in childbirth, compared with no headache, was associated with a small but statistically significant absolute increase in the risk of being diagnosed with intracranial subdural hematoma. Further research is needed to establish if this association is causal for this rare outcome.
中文翻译:

分娩后神经麻醉后硬膜穿刺后头痛与颅内硬膜下血肿的关系。
重要性 分娩的妇女在神经麻醉后继发硬脑膜穿刺的发生率很高,极有可能导致头痛。硬膜外穿刺后头痛与随后的颅内硬膜下血肿之间是否存在显着相关性似乎是未知的。
目的 探讨硬膜外穿刺头痛与产后颅内硬膜下血肿的关系。
设计,地点和参与者 这项队列研究使用了美国医疗保健研究与质量国家再入院数据库中记录的2010年1月至2016年12月分娩的妇女的医院出院患者。如果已入院,则包括这些患者,有2个月的随访数据,并且未接受诊断性腰穿。仅研究一个日历年的首次交付。分析了2018年1月至2019年6月的数据。
暴露 使用国际疾病分类(第9版和第10版)代码识别在产后2个月内发生神经硬膜外麻醉并伴有硬脑膜穿刺头痛的妇女,并将其与没有硬脑膜穿刺后头痛的妇女进行比较。
主要结果和措施 主要结果是产后2个月内颅内硬膜下血肿。次要结果包括院内死亡率和神经外科手术的发生。
结果 总共包括26 469 771例患者,分娩26 498 194例。排除重复分娩(n = 28 423),不进行2个月随访数据的分娩(n = 4 329 621)和诊断性腰椎穿刺的分娩(n = 9334),最终队列为22130815例患者,交付。对于该队列,平均(SD)年龄为28.1(6.0)岁,硬脊膜穿刺后头痛为68374,每10万人的总发生率为309(95%CI,302-316)。342确定硬膜下血肿的病例,每10万名女性中有1.5例发生率(95%CI,1.3-1.8)。在这些病例中,有100例是患有硬脑膜穿刺后头痛的女性,这表明该亚组中每10万分娩中有147例(95%CI,111-194)血肿病例。硬膜外穿刺后头痛的未调整绝对风险增加145(95%CI,117-174)每十万分娩的硬膜下血肿病例。调整混杂因素后,硬膜下穿刺头痛的硬膜下血肿比值比为199(95%CI,126-317;P <.001),且 每十万次分娩的调整后绝对风险增加130(95%CI,90-169; P <.001)。
结论与相关性 与无头痛相比,分娩后神经麻醉后硬脑膜穿刺后头痛的存在与确诊颅内硬膜下血肿的风险有绝对的微小增加,但在统计学上显着相关。需要进一步的研究来确定这种关联是否是这种罕见结果的原因。











































 京公网安备 11010802027423号
京公网安备 11010802027423号