JACC: Heart Failure ( IF 10.3 ) Pub Date : 2019-09-11 , DOI: 10.1016/j.jchf.2019.04.018 Jonathan G Howlett 1 , Amanda Stebbins 2 , Mark C Petrie 3 , Pardeep S Jhund 3 , Serenella Castelvecchio 4 , Alexander Cherniavsky 5 , Carla A Sueta 6 , Ambuj Roy 7 , Ileana L Piña 8 , Raphael Wurm 9 , Mark H Drazner 10 , Bert Andersson 11 , Carmen Batlle 12 , Michele Senni 13 , Lukasz Chrzanowski 14 , Bela Merkely 15 , Peter Carson 16 , Patrice M Desvigne-Nickens 17 , Kerry L Lee 2 , Eric J Velazquez 18 , Hussein R Al-Khalidi 2 ,
|
Objectives
The authors investigated the impact of coronary artery bypass grafting (CABG) on first and recurrent hospitalization in this population.
Background
In the STICH (Surgical Treatment for Ischemic Heart Failure) trial, CABG reduced all-cause death and hospitalization in patients with and ischemic cardiomyopathy and left ventricular ejection fraction <35%.
Methods
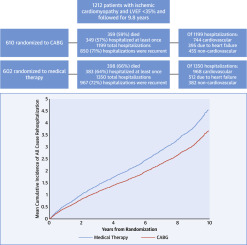
A total of 1,212 patients were randomized (610 to CABG + optimal medical therapy [CABG] and 602 to optimal medical therapy alone [MED] alone) and followed for a median of 9.8 years. All-cause and cause-specific hospitalizations were analyzed as time-to-first-event and as recurrent event analysis.
Results
Of the 1,212 patients, 757 died (62.4%) and 732 (60.4%) were hospitalized at least once, for a total of 2,549 total all-cause hospitalizations. Most hospitalizations (66.2%) were for cardiovascular causes, of which approximately one-half (907 or 52.9%) were for heart failure. More than 70% of all hospitalizations (1,817 or 71.3%) were recurrent events. The CABG group experienced fewer all-cause hospitalizations in the time-to-first-event (349 CABG vs. 383 MED, adjusted hazard ratio [HR]: 0.85; 95% confidence interval [CI]: 0.74 to 0.98; p = 0.03) and in recurrent event analyses (1,199 CABG vs. 1,350 MED, HR: 0.78, 95% CI: 0.65 to 0.94; p < 0.001). This was driven by fewer total cardiovascular (CV) hospitalizations (744 vs. 968; p < 0.001, adjusted HR: 0.66, 95% CI: 0.55 to 0.81; p = 0.001), the majority of which were due to HF (395 vs. 512; p < 0.001, adjusted HR: 0.68, 95% CI: 0.52-0.89; p = 0.005). We did not observe a difference in non-CV events.
Conclusions
CABG reduces all-cause, CV, and HF hospitalizations in time-to-first-event and recurrent event analyses. (Comparison of Surgical and Medical Treatment for Congestive Heart Failure and Coronary Artery Disease [STICH]; NCT00023595)
中文翻译:

CABG 改善缺血性心肌病患者的预后:STICH 试验的 10 年随访。
目标
作者调查了冠状动脉旁路移植术(CABG)对该人群首次和再次住院的影响。
背景
在 STICH(缺血性心力衰竭的手术治疗)试验中,CABG 减少了缺血性心肌病患者的全因死亡和住院治疗,左心室射血分数为 <35%。
方法
共有 1,212 名患者被随机分配(610 名患者接受 CABG + 最佳药物治疗 [CABG],602 名患者接受单独最佳药物治疗 [MED]),随访中位时间为 9.8 年。全因和特定原因住院治疗按首次事件发生时间和复发事件分析进行分析。
结果
在 1,212 名患者中,757 名患者死亡(62.4%),732 名患者(60.4%)至少住院一次,总计 2,549 名全因住院患者。大多数住院 (66.2%) 是因心血管原因,其中大约一半 (907 或 52.9%) 是因心力衰竭。超过 70% 的住院治疗(1,817 例或 71.3%)是复发事件。 CABG 组在首次事件发生期间因全因住院的情况较少(349 例 CABG 与 383 例 MED,调整后风险比 [HR]:0.85;95% 置信区间 [CI]:0.74 至 0.98;p = 0.03 )和复发事件分析(1,199 CABG vs. 1,350 MED,HR:0.78,95% CI:0.65 至 0.94;p < 0.001)。这是由于心血管 (CV) 住院总数减少(744 例 vs. 968 例;p < 0.001,调整后 HR:0.66,95% CI:0.55 至 0.81;p = 0.001),其中大部分是由于心力衰竭(395与 512 相比;p < 0.001,调整后 HR:0.68,95% CI:0.52-0.89;p = 0.005)。我们没有观察到非 CV 事件的差异。
结论
在首次事件发生时间和复发事件分析中,CABG 减少了全因、心血管和心力衰竭住院率。 (充血性心力衰竭和冠状动脉疾病的手术与药物治疗的比较 [STICH];NCT00023595)











































 京公网安备 11010802027423号
京公网安备 11010802027423号