JACC: Heart Failure ( IF 10.3 ) Pub Date : 2019-08-26 , DOI: 10.1016/j.jchf.2019.06.003 Inge Schjødt 1 , Søren P Johnsen 2 , Anna Strömberg 3 , Nickolaj R Kristensen 4 , Brian B Løgstrup 5
|
Objectives
This study examined the associations between socioeconomic factors (SEF), readmission, and mortality in patients with incident heart failure (HF) with reduced ejection fraction (HFrEF) in a tax-financed universal health care system.
Background
Lack of health insurance is considered a key factor in health inequality, leading to poor clinical outcomes. However, data are sparse for the association between SEF and clinical outcomes among patients with HF in countries with tax-financed health care systems.
Methods
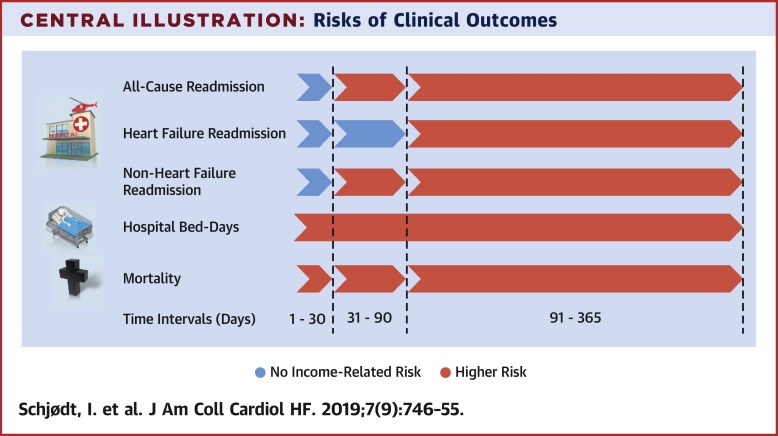
A nationwide population-based cohort study of 17,122 patients with incident HFrEF was carried out. Associations were assessed between individual-level SEF (cohabitation status, education, and income) and all-cause, HF, and non-HF readmission and mortality within 1 to 30, 31 to 90, and 91 to 365 days, as well as hospital bed days within 1 year after HF diagnosis.
Results
Low income was associated with a higher risk of all-cause readmission (adjusted hazard ratio [HR]: 1.24; 95% confidence interval [CI]: 1.08 to 1.43) and non-HF readmission (HR: 1.36; 95% CI: 1.17 to 1.58) within days 31 to 90 as well as with a higher risk of all-cause (HR: 1.27; 95% CI: 1.14 to 1.41), HF (HR: 1.26; 95% CI: 1.02 to 1.55) and non-HF readmission (HR: 1.25; 95% CI: 1.12 to 1.39) within days 91 to 365. Low-income patients also had a higher use of hospital bed days and risk of mortality during follow-up.
Conclusions
In a tax-financed universal health care system, low income was associated with a higher risk of all-cause and non-HF readmission within 1 to 12 months after HF diagnosis and with HF readmission within 3 to 12 months among patients with incident HFrEF. Low-income patients also had a higher number of hospital bed days and a higher rate of mortality during follow-up.
中文翻译:

全民医疗保健系统中心力衰竭患者的社会经济因素和临床结果。
目标
这项研究检查了在税收资助的全民医疗保健系统中射血分数降低(HFrEF)的突发性心力衰竭(HF)患者的社会经济因素(SEF),再入院率和死亡率之间的关联。
背景
缺乏健康保险被认为是造成健康不平等的关键因素,从而导致不良的临床结果。但是,在有税收资助的卫生保健系统的国家中,HF患者的SEF与临床结局之间的关联性数据很少。
方法
在全国范围内对17,122例HFrEF事件进行了队列研究。在个人级别的SEF(同居状态,教育和收入)与全因,HF和非HF再入院率和死亡率之间的关联性进行了评估,范围为1至30天,31至90天和91至365天,以及医院HF诊断后一年内的卧床天数。
结果
低收入与全因再入院的风险较高(调整后的危险比[HR]:1.24; 95%置信区间[CI]:1.08至1.43)和非HF再入院(HR:1.36; 95%CI:1.17)在31至90天之内达到1.58),并且全因风险较高(HR:1.27; 95%CI:1.14至1.41),HF(HR:1.26; 95%CI:1.02至1.55)和非HF在91至365天内再次入院(HR:1.25; 95%CI:1.12至1.39)。低收入患者的病床使用天数也较高,且在随访期间有死亡风险。
结论
在税收资助的全民医疗保健系统中,低收入与HF诊断后1至12个月内全因和非HF再入院的风险较高以及HFrEF事件患者在3至12个月内再次入院有关。低收入患者在随访期间的病床天数也更高,死亡率更高。











































 京公网安备 11010802027423号
京公网安备 11010802027423号