当前位置:
X-MOL 学术
›
npj Digit. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
City-wide electronic health records reveal gender and age biases in administration of known drug-drug interactions.
npj Digital Medicine ( IF 15.2 ) Pub Date : 2019-07-23 , DOI: 10.1038/s41746-019-0141-x Rion Brattig Correia 1, 2, 3 , Luciana P de Araújo Kohler 4 , Mauro M Mattos 4 , Luis M Rocha 1, 3
npj Digital Medicine ( IF 15.2 ) Pub Date : 2019-07-23 , DOI: 10.1038/s41746-019-0141-x Rion Brattig Correia 1, 2, 3 , Luciana P de Araújo Kohler 4 , Mauro M Mattos 4 , Luis M Rocha 1, 3
Affiliation
|
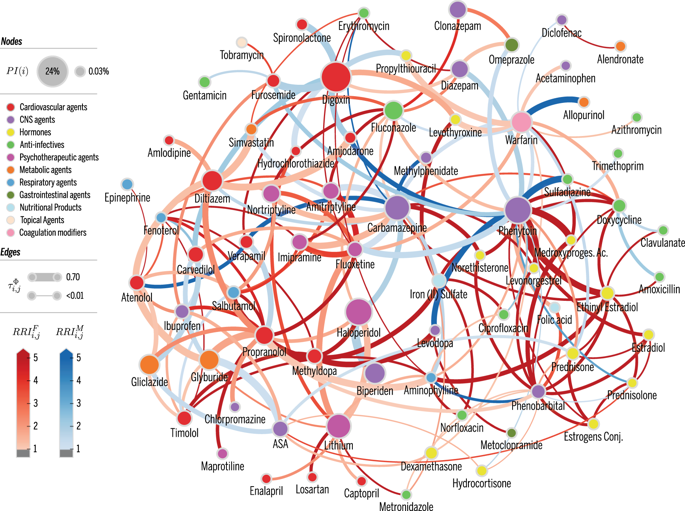
The occurrence of drug-drug-interactions (DDI) from multiple drug dispensations is a serious problem, both for individuals and health-care systems, since patients with complications due to DDI are likely to reenter the system at a costlier level. We present a large-scale longitudinal study (18 months) of the DDI phenomenon at the primary- and secondary-care level using electronic health records (EHR) from the city of Blumenau in Southern Brazil (pop. ≈340,000). We found that 181 distinct drug pairs known to interact were dispensed concomitantly to 12% of the patients in the city's public health-care system. Further, 4% of the patients were dispensed drug pairs that are likely to result in major adverse drug reactions (ADR)-with costs estimated to be much larger than previously reported in smaller studies. The large-scale analysis reveals that women have a 60% increased risk of DDI as compared to men; the increase becomes 90% when considering only DDI known to lead to major ADR. Furthermore, DDI risk increases substantially with age; patients aged 70-79 years have a 34% risk of DDI when they are dispensed two or more drugs concomitantly. Interestingly, a statistical null model demonstrates that age- and female-specific risks from increased polypharmacy fail by far to explain the observed DDI risks in those populations, suggesting unknown social or biological causes. We also provide a network visualization of drugs and demographic factors that characterize the DDI phenomenon and demonstrate that accurate DDI prediction can be included in health care and public-health management, to reduce DDI-related ADR and costs.
中文翻译:

全市范围内的电子健康记录揭示了已知药物-药物相互作用管理中的性别和年龄偏见。
对于个人和卫生保健系统而言,由于多种药物分配产生的药物相互作用(DDI)都是一个严重的问题,因为患有DDI并发症的患者很可能会以更高的价格重新进入系统。我们使用来自巴西南部布鲁曼瑙市的电子健康记录(EHR),对初级和二级医疗水平的DDI现象进行了大规模的纵向研究(18个月)(人口约340,000)。我们发现,该市的公共卫生保健系统中有181种不同的已知药物对同时被分配给了12%的患者。此外,有4%的患者分配了可能导致重大药物不良反应(ADR)的配药对-费用估计比以前在较小的研究中报道的要大得多。大规模分析表明,与男性相比,女性罹患DDI的风险增加了60%;如果仅考虑已知会导致主要ADR的DDI,则增加幅度为90%。此外,DDI风险会随着年龄的增长而大大增加;年龄在70-79岁之间的患者在同时分配两种或两种以上药物时有34%的DDI风险。有趣的是,一个统计无效模型表明,由于混合药店的增加,特定于年龄和女性的风险远远不能解释在这些人群中观察到的DDI风险,暗示了未知的社会或生物学原因。我们还提供了代表DDI现象特征的药物和人口统计因素的网络可视化,并证明了可以在医疗保健和公共卫生管理中包括准确的DDI预测,以减少与DDI相关的ADR和成本。
更新日期:2019-11-18
中文翻译:

全市范围内的电子健康记录揭示了已知药物-药物相互作用管理中的性别和年龄偏见。
对于个人和卫生保健系统而言,由于多种药物分配产生的药物相互作用(DDI)都是一个严重的问题,因为患有DDI并发症的患者很可能会以更高的价格重新进入系统。我们使用来自巴西南部布鲁曼瑙市的电子健康记录(EHR),对初级和二级医疗水平的DDI现象进行了大规模的纵向研究(18个月)(人口约340,000)。我们发现,该市的公共卫生保健系统中有181种不同的已知药物对同时被分配给了12%的患者。此外,有4%的患者分配了可能导致重大药物不良反应(ADR)的配药对-费用估计比以前在较小的研究中报道的要大得多。大规模分析表明,与男性相比,女性罹患DDI的风险增加了60%;如果仅考虑已知会导致主要ADR的DDI,则增加幅度为90%。此外,DDI风险会随着年龄的增长而大大增加;年龄在70-79岁之间的患者在同时分配两种或两种以上药物时有34%的DDI风险。有趣的是,一个统计无效模型表明,由于混合药店的增加,特定于年龄和女性的风险远远不能解释在这些人群中观察到的DDI风险,暗示了未知的社会或生物学原因。我们还提供了代表DDI现象特征的药物和人口统计因素的网络可视化,并证明了可以在医疗保健和公共卫生管理中包括准确的DDI预测,以减少与DDI相关的ADR和成本。



























 京公网安备 11010802027423号
京公网安备 11010802027423号