Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Causes of severe pneumonia requiring hospital admission in children without HIV infection from Africa and Asia: the PERCH multi-country case-control study.
The Lancet ( IF 98.4 ) Pub Date : 2019-06-27 , DOI: 10.1016/s0140-6736(19)30721-4 Katherine L. O'Brien , Henry C. Baggett , W. Abdullah Brooks , Daniel R. Feikin , Laura L. Hammitt , Melissa M. Higdon , Stephen R.C. Howie , Maria Deloria Knoll , Karen L. Kotloff , Orin S. Levine , Shabir A. Madhi , David R. Murdoch , Christine Prosperi , J. Anthony G. Scott , Qiyuan Shi , Donald M. Thea , Zhenke Wu , Scott L. Zeger , Peter V. Adrian , Pasakorn Akarasewi , Trevor P. Anderson , Martin Antonio , Juliet O. Awori , Vicky L. Baillie , Charatdao Bunthi , James Chipeta , Mohammod Jobayer Chisti , Jane Crawley , Andrea N. DeLuca , Amanda J. Driscoll , Bernard E. Ebruke , Hubert P. Endtz , Nicholas Fancourt , Wei Fu , Doli Goswami , Michelle J. Groome , Meredith Haddix , Lokman Hossain , Yasmin Jahan , E. Wangeci Kagucia , Alice Kamau , Ruth A. Karron , Sidi Kazungu , Nana Kourouma , Locadiah Kuwanda , Geoffrey Kwenda , Mengying Li , Eunice M. Machuka , Grant Mackenzie , Nasreen Mahomed , Susan A. Maloney , Jessica L. McLellan , Joanne L. Mitchell , David P. Moore , Susan C. Morpeth , Azwifarwi Mudau , Lawrence Mwananyanda , James Mwansa , Micah Silaba Ominde , Uma Onwuchekwa , Daniel E. Park , Julia Rhodes , Pongpun Sawatwong , Phil Seidenberg , Arifin Shamsul , Eric A.F. Simões , Seydou Sissoko , Somwe Wa Somwe , Samba O. Sow , Mamadou Sylla , Boubou Tamboura , Milagritos D. Tapia , Somsak Thamthitiwat , Aliou Toure , Nora L. Watson , Khalequ Zaman , Syed M.A. Zaman
The Lancet ( IF 98.4 ) Pub Date : 2019-06-27 , DOI: 10.1016/s0140-6736(19)30721-4 Katherine L. O'Brien , Henry C. Baggett , W. Abdullah Brooks , Daniel R. Feikin , Laura L. Hammitt , Melissa M. Higdon , Stephen R.C. Howie , Maria Deloria Knoll , Karen L. Kotloff , Orin S. Levine , Shabir A. Madhi , David R. Murdoch , Christine Prosperi , J. Anthony G. Scott , Qiyuan Shi , Donald M. Thea , Zhenke Wu , Scott L. Zeger , Peter V. Adrian , Pasakorn Akarasewi , Trevor P. Anderson , Martin Antonio , Juliet O. Awori , Vicky L. Baillie , Charatdao Bunthi , James Chipeta , Mohammod Jobayer Chisti , Jane Crawley , Andrea N. DeLuca , Amanda J. Driscoll , Bernard E. Ebruke , Hubert P. Endtz , Nicholas Fancourt , Wei Fu , Doli Goswami , Michelle J. Groome , Meredith Haddix , Lokman Hossain , Yasmin Jahan , E. Wangeci Kagucia , Alice Kamau , Ruth A. Karron , Sidi Kazungu , Nana Kourouma , Locadiah Kuwanda , Geoffrey Kwenda , Mengying Li , Eunice M. Machuka , Grant Mackenzie , Nasreen Mahomed , Susan A. Maloney , Jessica L. McLellan , Joanne L. Mitchell , David P. Moore , Susan C. Morpeth , Azwifarwi Mudau , Lawrence Mwananyanda , James Mwansa , Micah Silaba Ominde , Uma Onwuchekwa , Daniel E. Park , Julia Rhodes , Pongpun Sawatwong , Phil Seidenberg , Arifin Shamsul , Eric A.F. Simões , Seydou Sissoko , Somwe Wa Somwe , Samba O. Sow , Mamadou Sylla , Boubou Tamboura , Milagritos D. Tapia , Somsak Thamthitiwat , Aliou Toure , Nora L. Watson , Khalequ Zaman , Syed M.A. Zaman
|
BACKGROUND
Pneumonia is the leading cause of death among children younger than 5 years. In this study, we estimated causes of pneumonia in young African and Asian children, using novel analytical methods applied to clinical and microbiological findings.
METHODS
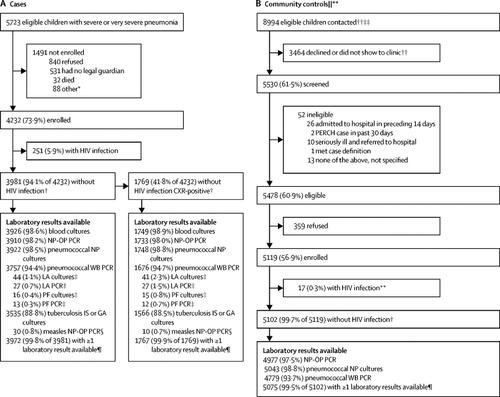
We did a multi-site, international case-control study in nine study sites in seven countries: Bangladesh, The Gambia, Kenya, Mali, South Africa, Thailand, and Zambia. All sites enrolled in the study for 24 months. Cases were children aged 1-59 months admitted to hospital with severe pneumonia. Controls were age-group-matched children randomly selected from communities surrounding study sites. Nasopharyngeal and oropharyngeal (NP-OP), urine, blood, induced sputum, lung aspirate, pleural fluid, and gastric aspirates were tested with cultures, multiplex PCR, or both. Primary analyses were restricted to cases without HIV infection and with abnormal chest x-rays and to controls without HIV infection. We applied a Bayesian, partial latent class analysis to estimate probabilities of aetiological agents at the individual and population level, incorporating case and control data.
FINDINGS
Between Aug 15, 2011, and Jan 30, 2014, we enrolled 4232 cases and 5119 community controls. The primary analysis group was comprised of 1769 (41·8% of 4232) cases without HIV infection and with positive chest x-rays and 5102 (99·7% of 5119) community controls without HIV infection. Wheezing was present in 555 (31·7%) of 1752 cases (range by site 10·6-97·3%). 30-day case-fatality ratio was 6·4% (114 of 1769 cases). Blood cultures were positive in 56 (3·2%) of 1749 cases, and Streptococcus pneumoniae was the most common bacteria isolated (19 [33·9%] of 56). Almost all cases (98·9%) and controls (98·0%) had at least one pathogen detected by PCR in the NP-OP specimen. The detection of respiratory syncytial virus (RSV), parainfluenza virus, human metapneumovirus, influenza virus, S pneumoniae, Haemophilus influenzae type b (Hib), H influenzae non-type b, and Pneumocystis jirovecii in NP-OP specimens was associated with case status. The aetiology analysis estimated that viruses accounted for 61·4% (95% credible interval [CrI] 57·3-65·6) of causes, whereas bacteria accounted for 27·3% (23·3-31·6) and Mycobacterium tuberculosis for 5·9% (3·9-8·3). Viruses were less common (54·5%, 95% CrI 47·4-61·5 vs 68·0%, 62·7-72·7) and bacteria more common (33·7%, 27·2-40·8 vs 22·8%, 18·3-27·6) in very severe pneumonia cases than in severe cases. RSV had the greatest aetiological fraction (31·1%, 95% CrI 28·4-34·2) of all pathogens. Human rhinovirus, human metapneumovirus A or B, human parainfluenza virus, S pneumoniae, M tuberculosis, and H influenzae each accounted for 5% or more of the aetiological distribution. We observed differences in aetiological fraction by age for Bordetella pertussis, parainfluenza types 1 and 3, parechovirus-enterovirus, P jirovecii, RSV, rhinovirus, Staphylococcus aureus, and S pneumoniae, and differences by severity for RSV, S aureus, S pneumoniae, and parainfluenza type 3. The leading ten pathogens of each site accounted for 79% or more of the site's aetiological fraction.
INTERPRETATION
In our study, a small set of pathogens accounted for most cases of pneumonia requiring hospital admission. Preventing and treating a subset of pathogens could substantially affect childhood pneumonia outcomes.
FUNDING
Bill & Melinda Gates Foundation.
中文翻译:

非洲和亚洲未感染艾滋病毒的儿童需要住院治疗的严重肺炎的原因:PERCH 多国病例对照研究。
背景肺炎是 5 岁以下儿童死亡的主要原因。在这项研究中,我们利用应用于临床和微生物学发现的新颖分析方法,估计了非洲和亚洲幼儿肺炎的病因。方法 我们在七个国家的九个研究点进行了一项多中心国际病例对照研究:孟加拉国、冈比亚、肯尼亚、马里、南非、泰国和赞比亚。所有研究中心都参加了为期 24 个月的研究。病例为因严重肺炎入院的1-59个月的儿童。对照组是从研究地点周围社区随机选择的年龄组匹配的儿童。通过培养物、多重 PCR 或两者同时检测鼻咽和口咽 (NP-OP)、尿液、血液、诱导痰、肺吸出物、胸水和胃吸出物。初步分析仅限于未感染 HIV 且胸部 X 光检查异常的病例以及未感染 HIV 的对照病例。我们应用贝叶斯、部分潜在类别分析来估计个体和人群水平上病因的概率,并结合病例和对照数据。结果 2011 年 8 月 15 日至 2014 年 1 月 30 日期间,我们登记了 4232 例病例和 5119 名社区对照者。主要分析组由 1769 例(4232 例中的 41·8%)未感染 HIV 且胸部 X 光检查呈阳性的病例和 5102 例(5119 例中的 99·7%)未感染 HIV 的社区对照组成。 1752 例中有 555 例 (31·7%) 存在喘息(按部位范围为 10·6-97·3%)。 30 天病死率为 6·4%(1769 例中有 114 例)。 1749 例中有 56 例 (3·2%) 血培养呈阳性,肺炎链球菌是最常见的分离细菌(56 例中有 19 例 [33·9%])。 几乎所有病例 (98·9%) 和对照 (98·0%) 的 NP-OP 标本中至少检测到一种病原体。 NP-OP 标本中呼吸道合胞病毒 (RSV)、副流感病毒、人偏肺病毒、流感病毒、肺炎链球菌、b 型流感嗜血杆菌 (Hib)、非 b 型流感嗜血杆菌和耶氏肺孢子菌的检测与病例状态相关。病原学分析估计,病毒占病因的 61·4%(95% 可信区间 [CrI] 57·3-65·6),细菌占 27·3%(23·3-31·6),分枝杆菌占 27·3%(23·3-31·6)。结核病为 5·9% (3·9-8·3)。病毒较少见(54·5%、95% CrI 47·4-61·5 vs 68·0%、62·7-72·7),细菌较常见(33·7%、27·2-40·) 8 vs 22·8%, 18·3-27·6) 极重症肺炎病例比重症病例高。 RSV 在所有病原体中的病因比例最高(31·1%,95% CrI 28·4-34·2)。人鼻病毒、人偏肺病毒A或B、人副流感病毒、肺炎链球菌、结核分枝杆菌和流感嗜血杆菌各占病原学分布的5%或更多。我们观察到百日咳博德特氏菌、副流感 1 型和 3 型、副肠病毒-肠道病毒、耶氏疟原虫、RSV、鼻病毒、金黄色葡萄球菌和肺炎链球菌的病原学分数按年龄划分的差异,以及 RSV、金黄色葡萄球菌、肺炎链球菌和肺炎链球菌严重程度的差异。副流感 3 型。每个地点的前 10 种病原体占该地点病原学分数的 79% 或更多。解释 在我们的研究中,一小部分病原体导致了大多数需要住院的肺炎病例。预防和治疗一部分病原体可能会极大地影响儿童肺炎的结局。资助比尔及梅琳达·盖茨基金会。
更新日期:2019-08-30
中文翻译:

非洲和亚洲未感染艾滋病毒的儿童需要住院治疗的严重肺炎的原因:PERCH 多国病例对照研究。
背景肺炎是 5 岁以下儿童死亡的主要原因。在这项研究中,我们利用应用于临床和微生物学发现的新颖分析方法,估计了非洲和亚洲幼儿肺炎的病因。方法 我们在七个国家的九个研究点进行了一项多中心国际病例对照研究:孟加拉国、冈比亚、肯尼亚、马里、南非、泰国和赞比亚。所有研究中心都参加了为期 24 个月的研究。病例为因严重肺炎入院的1-59个月的儿童。对照组是从研究地点周围社区随机选择的年龄组匹配的儿童。通过培养物、多重 PCR 或两者同时检测鼻咽和口咽 (NP-OP)、尿液、血液、诱导痰、肺吸出物、胸水和胃吸出物。初步分析仅限于未感染 HIV 且胸部 X 光检查异常的病例以及未感染 HIV 的对照病例。我们应用贝叶斯、部分潜在类别分析来估计个体和人群水平上病因的概率,并结合病例和对照数据。结果 2011 年 8 月 15 日至 2014 年 1 月 30 日期间,我们登记了 4232 例病例和 5119 名社区对照者。主要分析组由 1769 例(4232 例中的 41·8%)未感染 HIV 且胸部 X 光检查呈阳性的病例和 5102 例(5119 例中的 99·7%)未感染 HIV 的社区对照组成。 1752 例中有 555 例 (31·7%) 存在喘息(按部位范围为 10·6-97·3%)。 30 天病死率为 6·4%(1769 例中有 114 例)。 1749 例中有 56 例 (3·2%) 血培养呈阳性,肺炎链球菌是最常见的分离细菌(56 例中有 19 例 [33·9%])。 几乎所有病例 (98·9%) 和对照 (98·0%) 的 NP-OP 标本中至少检测到一种病原体。 NP-OP 标本中呼吸道合胞病毒 (RSV)、副流感病毒、人偏肺病毒、流感病毒、肺炎链球菌、b 型流感嗜血杆菌 (Hib)、非 b 型流感嗜血杆菌和耶氏肺孢子菌的检测与病例状态相关。病原学分析估计,病毒占病因的 61·4%(95% 可信区间 [CrI] 57·3-65·6),细菌占 27·3%(23·3-31·6),分枝杆菌占 27·3%(23·3-31·6)。结核病为 5·9% (3·9-8·3)。病毒较少见(54·5%、95% CrI 47·4-61·5 vs 68·0%、62·7-72·7),细菌较常见(33·7%、27·2-40·) 8 vs 22·8%, 18·3-27·6) 极重症肺炎病例比重症病例高。 RSV 在所有病原体中的病因比例最高(31·1%,95% CrI 28·4-34·2)。人鼻病毒、人偏肺病毒A或B、人副流感病毒、肺炎链球菌、结核分枝杆菌和流感嗜血杆菌各占病原学分布的5%或更多。我们观察到百日咳博德特氏菌、副流感 1 型和 3 型、副肠病毒-肠道病毒、耶氏疟原虫、RSV、鼻病毒、金黄色葡萄球菌和肺炎链球菌的病原学分数按年龄划分的差异,以及 RSV、金黄色葡萄球菌、肺炎链球菌和肺炎链球菌严重程度的差异。副流感 3 型。每个地点的前 10 种病原体占该地点病原学分数的 79% 或更多。解释 在我们的研究中,一小部分病原体导致了大多数需要住院的肺炎病例。预防和治疗一部分病原体可能会极大地影响儿童肺炎的结局。资助比尔及梅琳达·盖茨基金会。











































 京公网安备 11010802027423号
京公网安备 11010802027423号