当前位置:
X-MOL 学术
›
Prostate Cancer Prostatic. Dis.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Androgen decline and survival during docetaxel therapy in metastatic castration resistant prostate cancer (mCRPC).
Prostate Cancer and Prostatic Diseases ( IF 4.8 ) Pub Date : 2019-05-03 , DOI: 10.1038/s41391-019-0152-3 Charles J Ryan 1 , Sandipan Dutta 2 , William K Kelly 3 , Carly Russell 4 , Eric J Small 4 , Michael J Morris 5 , Mary-Ellen Taplin 6 , Susan Halabi 2 ,
Prostate Cancer and Prostatic Diseases ( IF 4.8 ) Pub Date : 2019-05-03 , DOI: 10.1038/s41391-019-0152-3 Charles J Ryan 1 , Sandipan Dutta 2 , William K Kelly 3 , Carly Russell 4 , Eric J Small 4 , Michael J Morris 5 , Mary-Ellen Taplin 6 , Susan Halabi 2 ,
Affiliation
|
BACKGROUND
Multiple androgens drive prostate cancer progression and higher pre-treatment levels of androgens, even within the castrate range, have been previously shown to be associated with an improved overall survival (OS) in mCRPC. Docetaxel impairs microtubules, has androgen receptor (AR) inhibitory effects and is used in both the castration resistant and sensitive settings, where androgen dynamics may impact outcome. The present analysis evaluates the association of decline in serum androgen levels (Testosterone (T), Androstenedione (A) and DHEA in docetaxel-treated mCRPC patients with OS.
METHODS
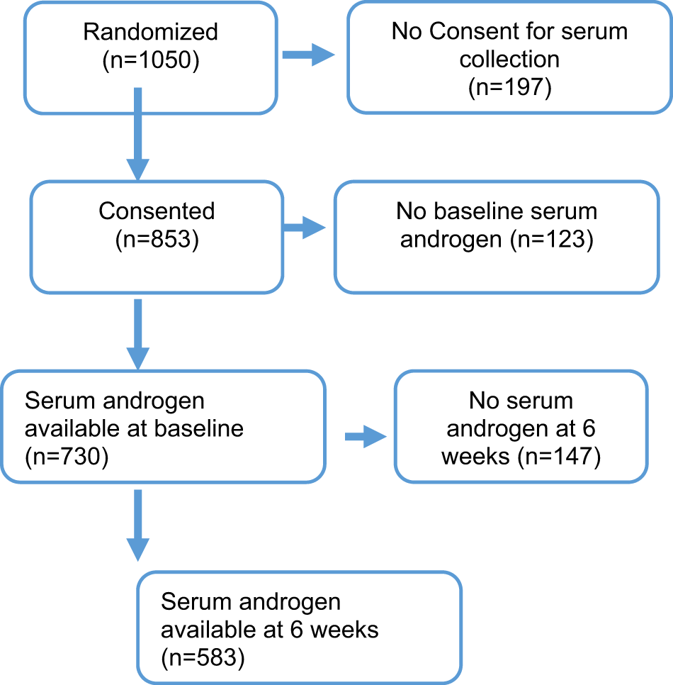
Data from 1050 men treated on CALGB 90401 with docetaxel, prednisone and either bevacizumab or placebo were evaluated. Eligibility required progressive mCRPC and no prior chemotherapy. Pre-treatment, 6 week and progression serum assays for T, A and DHEA were performed via tandem Liquid Chromatography-Mass Spectrometry (LC-MS/MS). Changes in T, A and DHEA levels from baseline to 6 weeks were calculated as the ratio of 6-week over baseline. The proportional hazards model was used to assess the prognostic significance of changes in T, A, and DHEA from baseline to 6 weeks in predicting OS adjusting for known prognostic factors.
RESULTS
Median baseline values for T, A, and, DHEA were 1.0, 13.5, and 8.1 ng/dL respectively while 6 week levels were 0.64, 7.0, and 6.8 ng/dL respectively. Median OS for low testosterone decline is 20.9 months vs 26.3 months for high testosterone decline. In multivariable analysis including known prognostic variables, change in testosterone levels was independently associated with greater OS; the hazard ratio for death with each unit increase in the 6-week/baseline ratio is 1.02 (95% CI = 1.01-1.03, p = 0.001). Decline in A and DHEA were not significant predictors of OS. In multivariable analysis change in the serum changes did not predict PFS however the ratio of T at 6-weeks over baseline was prognostic of ≥50% decline in PSA with an odds ratio of 0.93 (95% CI = 0.85-0.98, p-value = 0.039).
CONCLUSIONS
Declines in testosterone during docetaxel treatment is associated with a longer survival, consistent with a favorable prognostic significance of higher serum androgens in the CRPC.
中文翻译:

多西他赛治疗转移性去势抵抗性前列腺癌(mCRPC)期间雄激素的下降和存活率。
背景技术先前已显示多种雄激素驱动前列腺癌进展,并且甚至在去势率范围内更高水平的雄激素预处理水平与mCRPC的总体存活率(OS)的改善有关。多西紫杉醇可损害微管,具有雄激素受体(AR)抑制作用,可用于去势抵抗和敏感环境,其中雄激素动力学可能会影响结果。本分析评估了多西他赛治疗的OS的mCRPC患者中血清雄激素水平(睾丸激素(T),雄烯二酮(A)和DHEA)下降的相关性。方法1050名在CALGB 90401上接受多西他赛,强的松和贝伐单抗或评估安慰剂,是否需要进行渐进性mCRPC且无需事先化疗进行预处理,治疗6周和进行T血清测定,A和DHEA通过串联液相色谱-质谱(LC-MS / MS)进行。从基线到6周的T,A和DHEA水平的变化计算为基线6周的比率。使用比例风险模型评估从基线到6周的T,A和DHEA变化在预测OS对已知预后因素的调整中的预后意义。结果T,A和DHEA的中位基线值分别为1.0、13.5和8.1 ng / dL,而6周水平分别为0.64、7.0和6.8 ng / dL。睾丸激素低下者的OS中位数为20.9个月,而睾丸激素高下者为26.3个月。在包括已知预后变量在内的多变量分析中,睾丸激素水平的改变与更大的OS独立相关。每增加6周/基线比率,死亡的危险比为1.02(95%CI = 1.01-1.03,p = 0.001)。A和DHEA的下降不是OS的重要预测指标。在多变量分析中,血清变化的变化不能预测PFS,但是6周T值超过基线的比率预示了PSA下降≥50%,比值比为0.93(95%CI = 0.85-0.98,p值) = 0.039)。结论多西他赛治疗期间睾丸激素水平下降与更长的生存期相关,这与CRPC中较高的血清雄激素的有利预后意义相一致。在多变量分析中,血清变化的变化不能预测PFS,但是6周T值超过基线的比率预示了PSA下降≥50%,比值比为0.93(95%CI = 0.85-0.98,p值) = 0.039)。结论多西他赛治疗期间睾丸激素水平下降与更长的生存期相关,这与CRPC中较高的血清雄激素的有利预后意义相一致。在多变量分析中,血清变化的变化不能预测PFS,但是与基线相比6周时T的比率预示PSA下降≥50%,比值比为0.93(95%CI = 0.85-0.98,p值) = 0.039)。结论多西他赛治疗期间睾丸激素水平下降与更长的生存期相关,这与CRPC中较高的血清雄激素的有利预后意义相一致。
更新日期:2019-11-18
中文翻译:

多西他赛治疗转移性去势抵抗性前列腺癌(mCRPC)期间雄激素的下降和存活率。
背景技术先前已显示多种雄激素驱动前列腺癌进展,并且甚至在去势率范围内更高水平的雄激素预处理水平与mCRPC的总体存活率(OS)的改善有关。多西紫杉醇可损害微管,具有雄激素受体(AR)抑制作用,可用于去势抵抗和敏感环境,其中雄激素动力学可能会影响结果。本分析评估了多西他赛治疗的OS的mCRPC患者中血清雄激素水平(睾丸激素(T),雄烯二酮(A)和DHEA)下降的相关性。方法1050名在CALGB 90401上接受多西他赛,强的松和贝伐单抗或评估安慰剂,是否需要进行渐进性mCRPC且无需事先化疗进行预处理,治疗6周和进行T血清测定,A和DHEA通过串联液相色谱-质谱(LC-MS / MS)进行。从基线到6周的T,A和DHEA水平的变化计算为基线6周的比率。使用比例风险模型评估从基线到6周的T,A和DHEA变化在预测OS对已知预后因素的调整中的预后意义。结果T,A和DHEA的中位基线值分别为1.0、13.5和8.1 ng / dL,而6周水平分别为0.64、7.0和6.8 ng / dL。睾丸激素低下者的OS中位数为20.9个月,而睾丸激素高下者为26.3个月。在包括已知预后变量在内的多变量分析中,睾丸激素水平的改变与更大的OS独立相关。每增加6周/基线比率,死亡的危险比为1.02(95%CI = 1.01-1.03,p = 0.001)。A和DHEA的下降不是OS的重要预测指标。在多变量分析中,血清变化的变化不能预测PFS,但是6周T值超过基线的比率预示了PSA下降≥50%,比值比为0.93(95%CI = 0.85-0.98,p值) = 0.039)。结论多西他赛治疗期间睾丸激素水平下降与更长的生存期相关,这与CRPC中较高的血清雄激素的有利预后意义相一致。在多变量分析中,血清变化的变化不能预测PFS,但是6周T值超过基线的比率预示了PSA下降≥50%,比值比为0.93(95%CI = 0.85-0.98,p值) = 0.039)。结论多西他赛治疗期间睾丸激素水平下降与更长的生存期相关,这与CRPC中较高的血清雄激素的有利预后意义相一致。在多变量分析中,血清变化的变化不能预测PFS,但是与基线相比6周时T的比率预示PSA下降≥50%,比值比为0.93(95%CI = 0.85-0.98,p值) = 0.039)。结论多西他赛治疗期间睾丸激素水平下降与更长的生存期相关,这与CRPC中较高的血清雄激素的有利预后意义相一致。



























 京公网安备 11010802027423号
京公网安备 11010802027423号